Research assistant Hong Wang retrieves a small, clear, plastic tray from a stainless-steel incubator and places it carefully on the laboratory bench at Monash University’s Prostate Cancer Research Group.
And suddenly, there they are.
Tiny, pink slivers of live human tissue suspended in clear liquid, like floating bonito flakes. It’s almost anti-climactic. These are the source of my existential dread, the unravelling of my world over the past nine years? It hardly seems credible.
Not for the first time on this wild ride, managing a stage four, metastatic prostate cancer diagnosis, I ponder how I got here. More specifically, how I’ve ended up on this unlikely date with my nemesis. I don’t recall swiping right. Their profile looked awful. Red flags everywhere.
My 20-year marriage was just one of the casualties of my diagnosis and its brutal treatments. It was the late ’90s when I last dated, and the world has changed. I’ve changed. What to wear? How to make conversation? How to spot a narcissist? (I think cancer qualifies – so full of itself, so little room for anything else, endlessly taking up space, so oblivious to the suffering of others.)
This journey to meet my nemesis has brought me full circle. I grew up in the vast, flat, landlocked expanses of Melbourne‘s eastern suburbs in the ’70s – not the best start in life for a surfer and career surf journalist.
Nearly 40 years after I migrated north for balmier coastal climes, I’m again traversing this familiar landscape. Suburbia has endlessly replicated itself here, on the road to the University’s Clayton campus, spreading ever outwards, encroaching into green spaces, arterial roads stretching like tentacles into former farmlands.
And yet for me there’s a warm glow of nostalgia as all those squat, triple-fronted, brick-veneer homes and soulless new housing estates, Melbourne’s ubiquitous milk bars, and fish and chip shops whizz by out the windows of my mum’s Honda Jazz.
Golden memories of suburban footy matches, Friday-night hang-outs at the local shopping centre, sculled Lilydale cider or cask wine, late-night steamed dim sims, first kisses and other teen intrigues.
Here I am, now 59, nine years after my diagnosis, still – astonishingly – not just alive, but fit and healthy, returning home for a surprising new work gig – a research fellow reporting on prostate cancer research.

Fragile rogues
Professor Gail Risbridger (AM) has an unrivalled knowledge of hormonal cancers and the tricky business of keeping cancer cells alive in the lab. This skillset, and a staunch fearlessness to stake her ground in a male-dominated field, led to the formation of this group.
After reading my memoir of my cancer diagnosis, Patting the Shark, Professor Risbridger invited me aboard this hub of cutting-edge medical research.
Today is my first day on the tools, and in the lab, at Monash University’s School of Biomedical Sciences, and a face-to-face appointment with the small clusters of rogue cells that have threatened my life.
The Monash group has one of the largest collections of live prostate cancer cells in the world. Many have outlived the men who donated them, carefully retrieved from biopsies, radical prostatectomies (the surgical removal of a cancerous prostate), or donated to medical science upon their owner’s death.
This collection, known as MURAL (Melbourne Urology Research Alliance), has assisted the research of scientists globally.
These live cancer cells make it possible to test numerous treatments at once and in varying combinations, until the more promising treatments have passed the many hurdles to move on to human trials.
Prostate cancer is now Australia’s most common form of cancer, having recently overtaken breast cancer. In this country, one in six men will be diagnosed with this cancer. There were 22,000 new cases diagnosed in 2022 and 3500 deaths.
Ironically, these rogue cells, which wreak such havoc and are so difficult to eradicate in the human body, are extraordinarily fragile and challenging to keep alive outside of it. We are, biologically, the perfect hosts.
Meeting the unseen enemy
To meet these cells, the unseen enemy within that has so profoundly upended my life, I make my way towards the biomedicine school down the aptly named Innovation Walk, a wide pedestrian boulevard lined with towering gum trees. I’m surprisingly calm, with just a hint of frisson, hoping the date goes well.
I find Professor Risbridger on the third floor, at her desk working on a thesis that attempts to capture the multitudinous highlights of her life’s work: “Hormones in development and diseases of the male – a collection of published works from 1980 to 2024.” A kind of greatest-hits album from an illustrious scientific career.
Gail and I have met several times before, at medical conferences and for coffee catch-ups and Zoom calls. For the past couple of years, I’ve played a role as a “consumer voice” or patient representative on several research grant applications, a requirement to ensure the patient experience informs their research focus.
On my first visit here in that role a year ago, I was moved by how warmly I was received – a living, breathing human face representing the patients whose lives these scientists are trying to save, the reason so many bright, brilliant minds are spending the best years of their lives hunched over microscopes and manipulating cancer cells.
Young, bright-eyed PhD students introduced themselves to me, eager to explain their research focus.
Once prostate cancer has spread beyond the prostate gland and migrated, or metastasised to the bone, as mine has, treatments are considered palliative, aiming to extend life rather than cure. And the frontline treatment of what’s euphemistically termed “hormone therapy”, or more bluntly known as chemical castration, comes with an alarming suite of debilitating side-effects.
I was delighted to learn that one of the Monash researchers’ recent grant applications had quoted a line about the effect of this therapy from my memoir:
“Discussing quality of life for men with prostate cancer while chemically castrating them is a little like recommending a good dentist while punching someone repeatedly in the face.”
These researchers saw my perspective on the travails of life on hormone therapy as an asset in making the case to fund research to find better and less-toxic treatments.
I’ve already experienced nine years of efficacy from the frontline treatment of hormone therapy, sometimes also known as androgen deprivation therapy. Most men get two to three years, before the cancer mutates and is considered “castrate resistant”, at which point the therapy becomes ineffective.
Living with advanced prostate cancer has been compared to being a frog on a lily pond. You stay on each lily pad until it can no longer support you, then hop to the next lily pad before you sink, and so on, hoping you don’t run out of lily pads. Prostate cancer researchers are tasked with developing new lily pads.
‘Rigour, reproducibility, accuracy’
Professor Risbridger’s special skill of keeping prostate cancer cells alive in the lab was developed in the ’90s during a Fulbright Scholarship at the University of California, San Francisco, under the mentorship of Professor Gerry Cunha, “a fantastic anatomist, teacher and musician”, she recalls.
She was at the forefront of the emerging field of stem cell research, and learnt to manipulate stem cells to become prostate cells. With a ready supply of both healthy and cancerous prostate cells, and an ability to keep them alive in the lab, she could study the drivers of growth in both.
“Understanding the mechanisms that control normal versus tumour growth from stem cells is crucial,” she says.
But the skillset to undertake this cutting-edge research was surprisingly domestic. Professor Risbridger recalls Professor Cunha asking her: “How good are you at sewing?”
“I said, ‘I do a lot of needlework and embroidery.’ He said, ‘You’ll probably be very good at this.’”
Far from taking offence at this gendered line of questioning, she saw the sense in it. “Hand-eye coordination is very critical, and good fine motor skills are needed to handle these delicate cells and tissues. Embroidery is about careful neatness.”
Read more: PSA testing for prostate cancer is only worth it for some
Stem cell research was a new and controversial area of research science in the ’90s, thrust into mainstream consciousness by Dolly the Sheep, the first mammal to be cloned from a cell taken from an adult mammal.
“Stem cells give rise to specialised cells such as bone, skin, teeth, prostate etc,” explains Professor Risbridger. “Until Dolly, we thought of it as a linear process – from stem cell to specialised cell … Dolly proved that wrong … You can manipulate a stem cell’s fate, and even reprogram specialised cells.”
This knowledge, combined with the ability to keep prostate cancer cells alive in the lab, was the breakthrough that would make the work of the group possible.
The other lucky break was then-US president George W. Bush’s prohibition of the emerging field of stem cell research on ethical grounds.
US prohibition became Australia’s opportunity. Professor Risbridger was funded by the US Department of Defence to work on prostate stem cells for over eight years. “It was exciting and completely serendipitous,” she says.
A combination of vision and pragmatism continues to drive Professor Risbridger’s research today. “What you want in science is rigour, reproducibility, accuracy,” she says, “because people want to be able to repeat what you do. Often the innovative is quite boutique and left-field.”
Delicate-looking intruders
After lunch, I’m handed into the care of Hong Wang, a member of the research support team who’s worked with Professor Risbridger for more than 25 years, part of the female-dominated workforce that has been attracted to the group.
Professor Risbridger believes this leads to a more cooperative, less hierarchical work culture, and female researchers have been drawn to work under a female mentor, even if it’s on a male disease.
Wang and I step into an antechamber between the offices and the lab, and don handsome blue smocks, hair nets and latex gloves. Wang retrieves the tray of prostate cancer samples from the incubator, carefully maintained at 37°C, the temperature of the human body, in an atmosphere composed of 5% CO₂, with a vessel of water at the bottom to maintain ideal humidity levels.
The tray is made up of a grid pattern of circular compartments, each the size of a five-cent piece, like a miniature ice cube tray. And in each compartment, suspended in a clear fluid, are live prostate cancer cells. Other samples are set in small mounds of clear gel, like well-organised pimples, which provides everything the cancer cells require to remain alive.
They look harmless and benign here in the lab, too small and frail to threaten human life, to invade the organs, bloodstream, and even bones of a grown man.
I stare ponderously. This is what all this fuss has been about? The endless cycles of blood tests and scans, chemotherapy infusions, targeted radiation, the long dark nights of the soul and existential terror.
The suppression of my testosterone cut off these mutant cells’ fuel supply and ability to grow and spread, leaving me depressed, sexless, at a higher risk of cardiovascular disease, diabetes, and even suicide.
Surely, I wonder, it must be possible to eradicate these delicate-looking intruders from the human body without making life feel almost unbearable for their unfortunate hosts.
The scientists here feel similarly and have devoted their lives to this quest. Current research projects include bipolar hormone therapy – that is, starving the body of testosterone, then hitting it with high doses of testosterone, which has the potential to “shock” the cancer into remission, while alleviating many of the side-effects of traditional hormone therapy.
But so far no one has been able to discern why this is effective in only about 30% of patients, while this therapy risks fuelling progression of the cancer in others.
Then there’s immunotherapy (empowering the body’s own immune system to recognise and fight cancer cells). So far this has proven elusive for prostate cancer because of its tendency to mutate and find ways around existing treatments. Identifying which patients might respond to immunotherapy and how it’s best-delivered remains an ongoing investigation here.
Tempting fate?
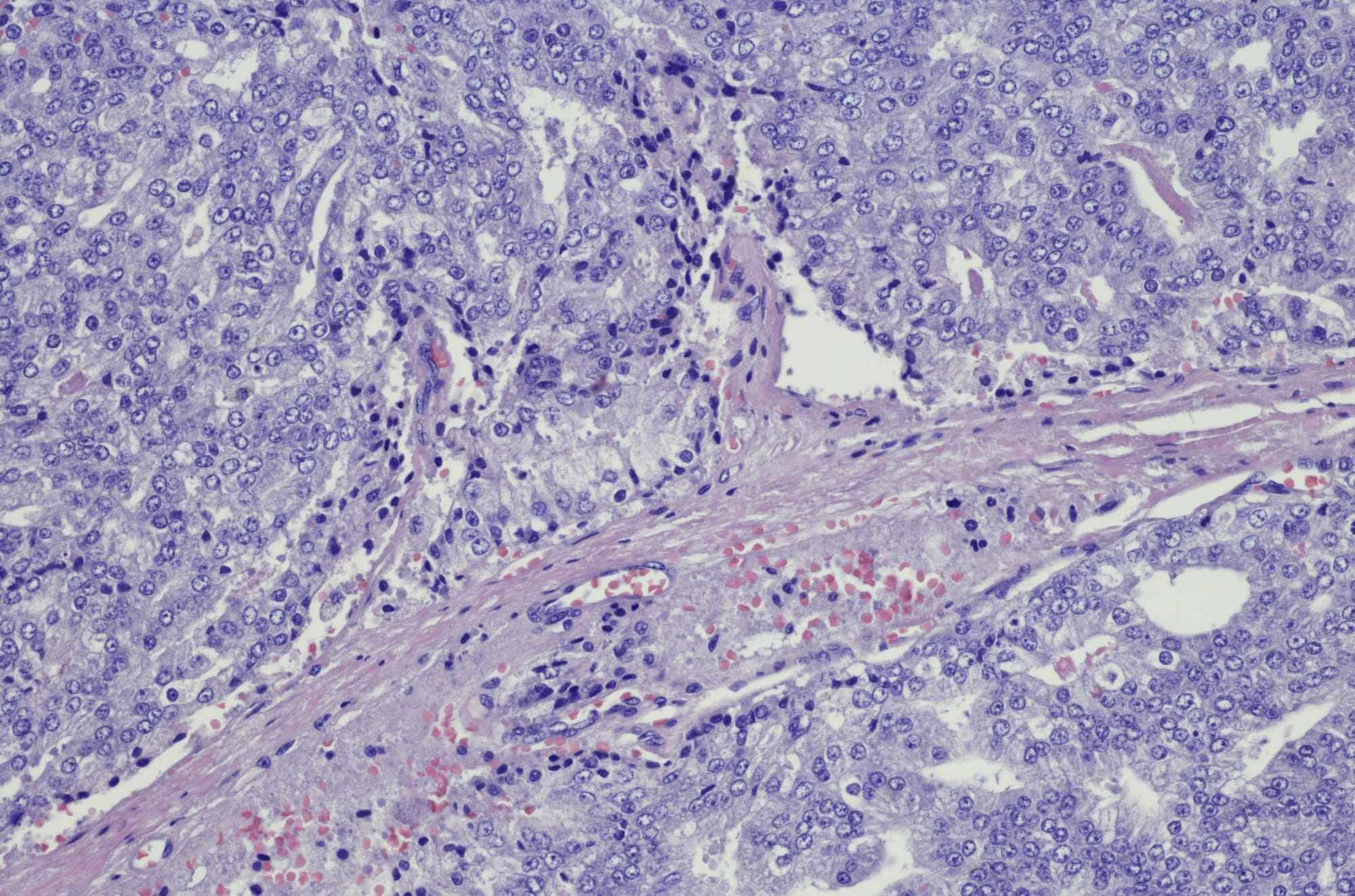
I’m invited to look at these live prostate cancer cells under the microscope, and suddenly they look less benign, more sinister. I squint to focus, and soon a foreboding, alien landscape reveals itself.
Healthy prostate cells look a little like the inside of a pomegranate, ordered, fairly uniform in shape and size and spacing.
Prostate cancer cells appear more haphazard, misshapen, clumped together randomly as they mutate and multiply without restraint.
The degree of chaos in the cells’ appearance reflects the aggressiveness of the cancer, and is measured by something called a Gleason Score. Mine registered an alarming nine out of 10 on diagnosis, which makes my continued good health even more surprising to my oncologist.

I wonder if I’m tempting fate with this close encounter, giving visual reality to a threat that has lain dormant for several years, giving me an unexpected reprieve. Let sleeping dogs lie, and all that.
On the other hand, meditation has become a major part of my self-care, and in more esoteric moments I dare to believe in a kind of magical thinking, that the striking visual appearance of these cells might allow me to imagine these untamed cells being corralled back into order and obedience. Not a lot of medical science at work here, though.
As I raise my eyes from the microscope, I’m snapped out of my metaphysical musings by the sterility of my environment. I’m a research fellow in a medical science lab, not a wellness guru extolling the power of the mind.
Still, I’m happy to have a bet each way. I’ll continue meditating, considering my cancer a teacher that can move on once the student has fully learned their lessons, in the hope of defying a prognosis I’ve already outlived by several years.
But I’m inordinately grateful someone’s doing the hard science of developing better treatment options.

Tim Baker works part-time as a research fellow for Monash University's Prostate Cancer Research Group.
This article originally appeared on The Conversation.





