As the global race to produce a vaccine against COVID-19 continues to heat up, researchers from the Peter Doherty Institute for Infection and Immunity and the Monash Institute for Pharmaceutical Sciences have developed two vaccine candidates that are providing encouraging results in preclinical testing.
The results have attracted almost $3 million in funding from the Commonwealth government’s Medical Research Future Fund (MRFF).
The approach focuses on the golf tee-shaped protein spikes that dot the surface of the SARS-Cov-2 virus.
The tip of the spike protein is known as the receptor binding domain (RBD), and is considered the most important target for antibodies produced by our immune systems, because this is the part of the virus that attaches to human cells.
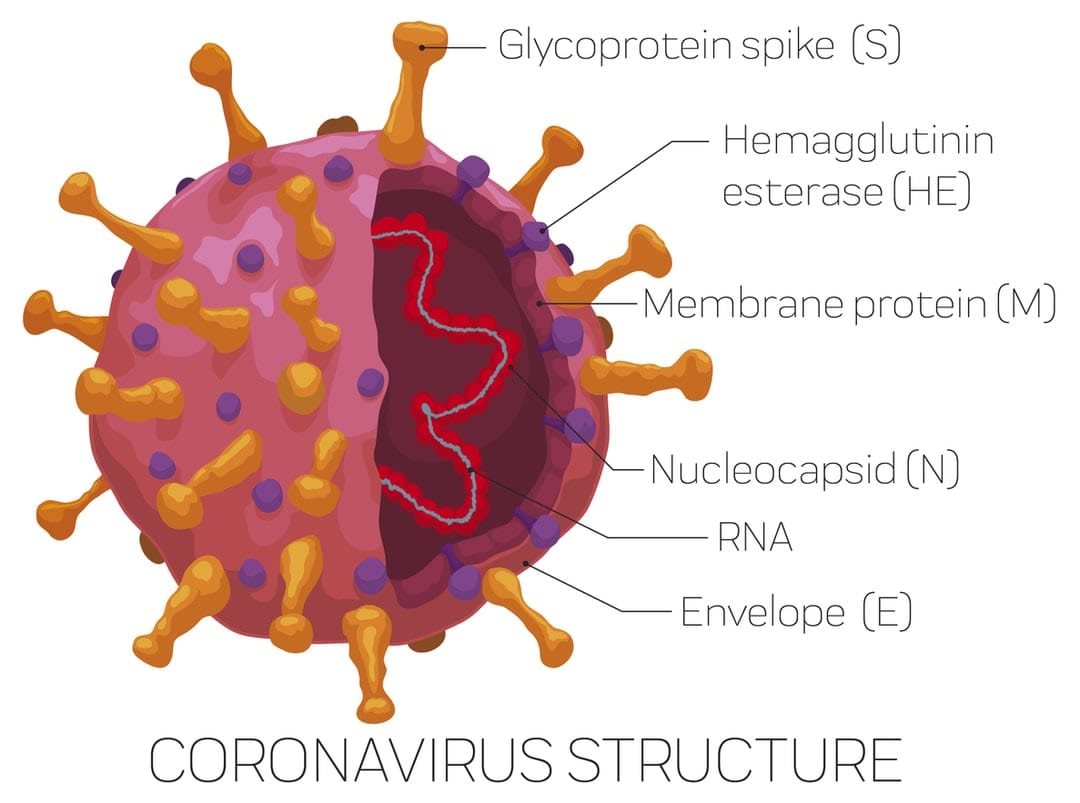
In effect, if you can block the attachment, you block the infection.
One of the vaccines isolates the molecular form of the RBD to focus the immune response on this critical region. The other includes messenger RNA (mRNA) to represent the genetic sequence of the virus, effectively tricking the immune system into thinking a virus is present so that it will make the antibodies.
Here, Monash University’s Professor Colin Pouton, who's working on the vaccine research projects, takes us behind the scenes of the process, and explains the importance of collaboration.
What is the potential vaccine you are trying to make, and how does it work? What makes it unique?
We’re delivering messenger RNA (mRNA) in common with some of the leading commercial programs. The mRNA contains the genetic code that allows our own cells to make part of the coronavirus spike protein. When our cells make the protein, our immune cells can recognise the protein as foreign, and this leads to production of antibodies.
The goal is to produce antibodies that bind to the virus and prevent infection. This is a new technology for vaccine development, but has a number of important advantages. mRNA can be produced quickly and, if the virus mutates, modified sequences can be produced rapidly. A cocktail of mRNA molecules could be used to hit several strains.
How did the collaboration with the Doherty Institute come about? What does the Doherty do well, and what does Monash do well?
We started working with virologists at the Doherty to analyse the quality of the immune response after vaccination of mice. The Doherty scientists can work with live virus, and can test whether our mouse antisera prevent infection using a cell culture infection model.
The Monash Institute of Pharmaceutical Sciences [MIPS] group includes specialists in mRNA production and formulation, but we don’t have specialised handling facilities to study viral infection and the immune responses to vaccines.
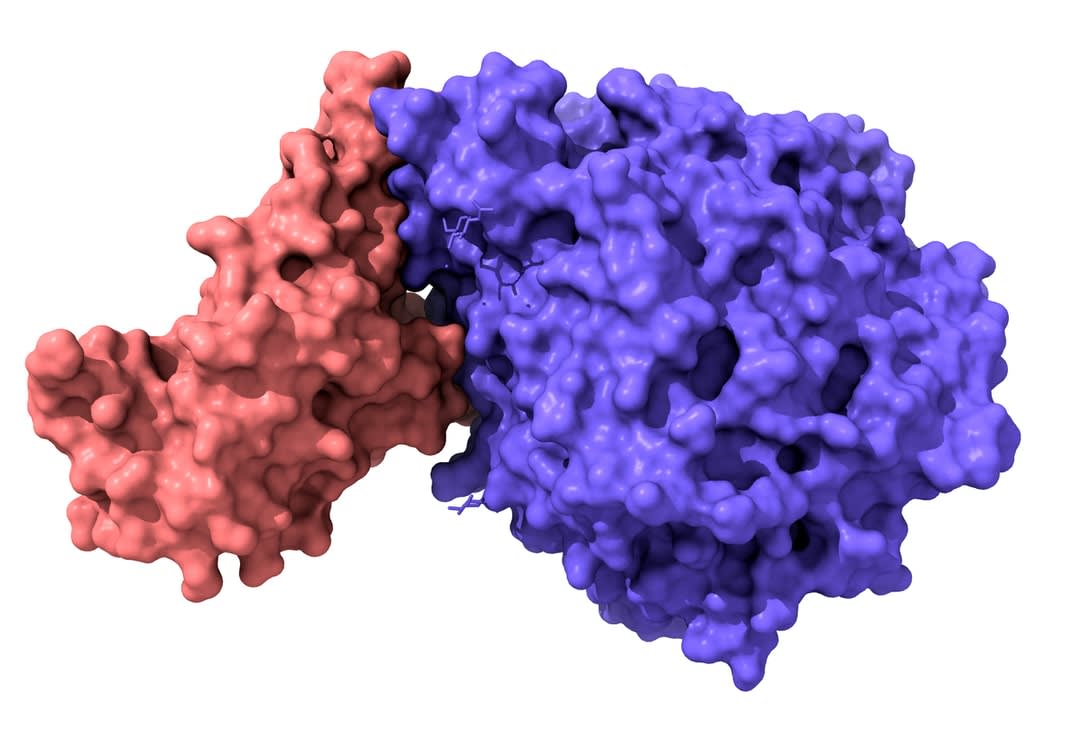
Later, we realised that the two groups shared an interest in producing vaccines focused on vaccinating with the receptor binding domain [RBD]. This is a small part of the spike protein, but neutralising antibodies need to bind to the RBD. So we’re now collaborating by investigating a protein developed by the Doherty group, as well as the mRNA developed by the MIPS group.
What’s the fundamental difference – and potential benefit – of the two institutes’ approaches to the virus?
The two vaccines – RBD protein from the Doherty, and mRNA encoding RBD from MIPS – offer an unusual opportunity to compare the attributes of the two delivery approaches head-to-head. We expect they’ll result in different responses.
Knowledge of how the vaccines differ will be valuable when designing the response to future emerging viruses.
Mostly we hear about the fierce competition between institutions and/or countries in vaccine development – how is this not the case here?
Collaborations work best when the individual parties bring different and complementary skills that make the case for collaboration compelling. The collaboration with the Doherty group is a good example. Competition between the institutions is not an option, because neither has all the required attributes.
In addition, I think the urgent need to respond to the COVID-19 pandemic has increased the willingness to collaborate.
What’s it been like working on a vaccine during serious pandemic lockdowns in Melbourne. How has it affected your lab work and work practices? Additionally, describe the MIPS team – how big is it, and who are they all?
The laboratory researchers have been able to work throughout the pandemic, but have been restricted by social distancing, reduced occupancy of the labs, and the need to wear masks all day. But the motivation is high, and the huge interest in vaccine development has been inspiring.
Read more: From Baghdad to Melbourne: Dr Harry Al-Wassiti's remarkable journey
The MIPS team is small. Harry Al-Wassiti has done much of the work, assisted by Estelle Suys and two PhD students, Asuka Takanashi and Tom Payne.
Was there a breakthrough moment in the science (from MIPS) that you can pinpoint for us?
Certainly – the proof that the mRNA vaccines we designed produced neutralising antibodies in mice was a key moment.
Has COVID-19 mutated since it emerged? Have you seen mutations in Melbourne, and what do mutations mean for your work? Does it mean a future vaccine might be seasonal, like a flu vax?
Virologists in Melbourne have been sequencing large numbers of viral isolates – greater than 5000 samples. There are lots of mutations – as would be expected for a RNA virus – but many of the mutations haven’t changed the threat of the virus.
Some mutations are significant. There’s been at least one mutation circulating in Victoria that binds more strongly to the known receptor (ACE2). This suggests that the vaccine design might need to adapt to mutations, and may need to be given in a seasonal manner. mRNA is particularly adaptable in this respect.
The big question – when might a vaccine be available, and what else is required to continue the work?
The leading commercial programs will complete their phase three trials within two to three months. If they’re safe and effective, the vaccines could be in use early in 2021.

The availability of vaccines in Australia will depend on the international capacity to produce doses, and whether they can be produced in Australia under licence. The Australian vaccines, if successful, will follow later – and the ability to take them forward into efficacy studies will depend on commercial partners and funding.
Outside of the two institutes (Monash and the Doherty Institute), is there something about the science community in Melbourne/Australia that has helped make this possible?
I arrived in Melbourne in 2001, and I’ve always found the environment to be highly collaborative. Proximity of the various universities and institutes in a large city is part of the reason. Also, there’s a lot of shared equipment, which fosters collaboration.
Finally, having looked at this novel coronavirus up closer than most, how would you describe it. What is it like?
The novel coronavirus is very closely related to other coronaviruses, and in particular to the SARS virus. Considering how close they are, there are surprising differences in how contagious each virus is, and how severe the disease caused.
It seems that severe coronavirus infections will be a continuing problem in the future. The pandemic has inspired a huge amount of research – just take a look at the BioRxiv platform for disseminating manuscripts prior to peer review. The number of relevant papers that have been published in six months is overwhelming – 8762 up to 17 September.