Despite incredible advances in reproductive technology, the World Health Organisation estimates that 48 million couples and 186 million individuals globally live with infertility.
The journey to conceiving a child can be an emotional and physical rollercoaster, often stressful and frustrating, and sometimes heartbreakingly without success.
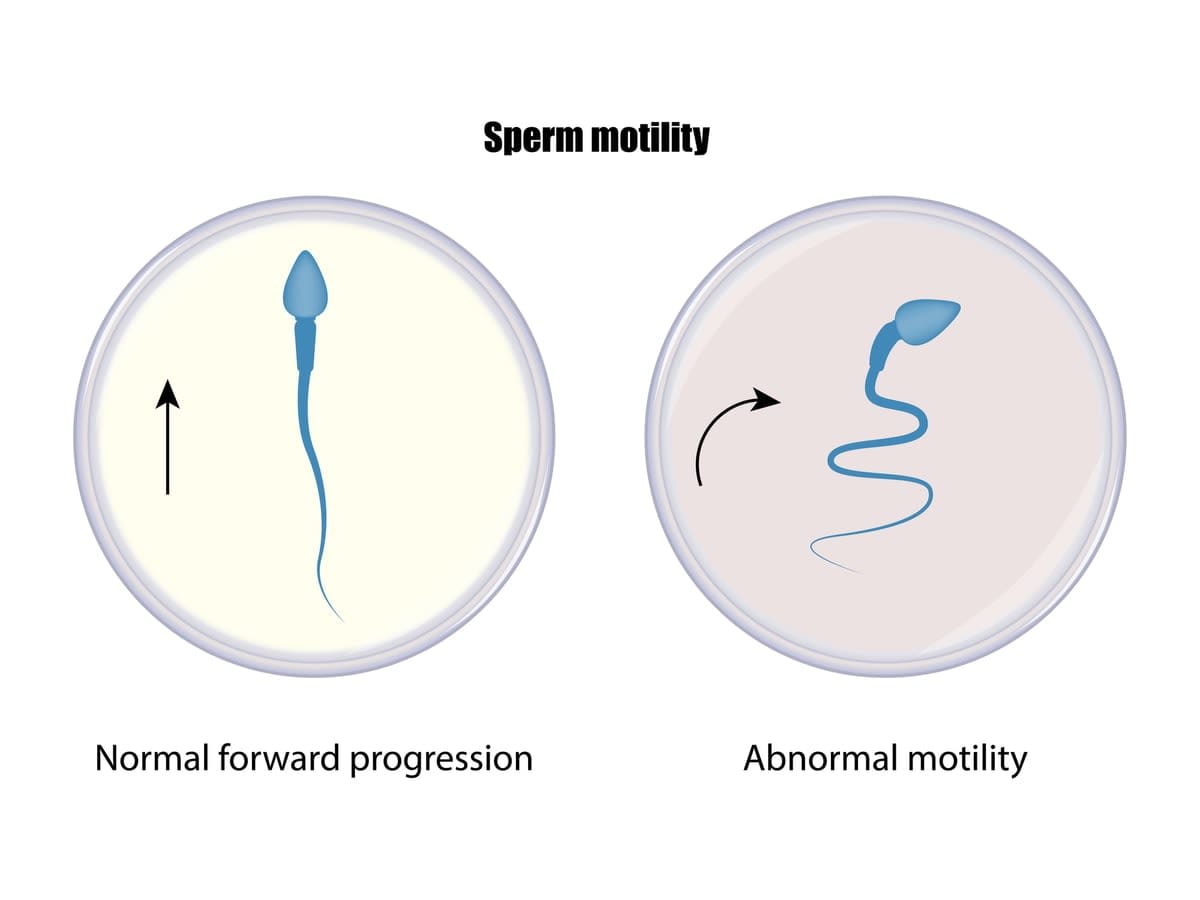
Generally, about 30% of infertility is due to low sperm motility – the inability of sperm to swim through the woman’s reproductive tract.
However, new research has found that using high-frequency ultrasound on sperm can boost their ability to swim.
Read more: Male fertility: The biological clock ticks for men, too, and affects IVF success
This breakthrough is another important piece in the jigsaw puzzle of fertility, offering new hope to those previously unable to conceive.
“This method will reduce the burden for couples experiencing infertility by either increasing the fertility rates in natural reproduction, or circumventing the need for more invasive interventions in assisted reproduction,” says Dr Reza Nosrati.
In a paper published in Advanced Science, and building on previous research, Dr Nosrati and colleagues Professor Adrian Neild and PhD student Junyang Gai, at Monash University’s Department of Mechanical and Aerospace Engineering, have shown how using acoustic-based mechanotherapy can improve sperm swimming ability at the single-cell level.
Ultrasound enhances metabolic activity
A healthy sperm has a lashing tail that helps it swim through the reproductive system. Sperm with poor motility may swim feebly or not at all.
“We’ve found that after just 20 seconds of high-frequency acoustic exposure, both the number of motile sperm in the sample and their swimming velocity increases by up to 30%, enhancing their ability to swim through the curved fallopian tube, without any adverse effects on sperm DNA integrity,” says Dr Nosrati.
Currently, the only other known method of inducing a twitching motility in sperm, to detect their viability or increase their swimming velocity, is an invasive treatment using the chemical pentoxifylline. However, cells treated this way quickly die.
Read more: Are chemicals shrinking your penis and depleting your sperm? Here's what the evidence really says
What we know so far is that high-frequency ultrasound improves sperm motility by enhancing the rate of its metabolic activity.
Sperm motility is produced by sperm flagellar beating, and an improvement in sperm motility is associated with a higher rate of energy production and its utilisation by the flagellum.
A mechanism known as ATP hydrolysis releases energy to drive dynein molecular motors along the flagellum and shape the flagellar waveform. Therefore, a change in the rate of energy production can influence sperm motility.
“We’re seeing impressive results of improvement in sperm motility only after five to 50 seconds of ultrasound exposure,” says Dr Nosrati.
“The great performance with short processing time enables this method to be easily integrated in the current clinical practices and workflow with minimal disruption.
“A sperm sample can be treated after collection during IVF procedures, and a portable platform for use in fertility clinics is currently in development.”
Dr Nosrati says this is a practical and relatively simple method of treating sperm, and envisions this as a kit sitting somewhere in the clinic, and just an extra step for the clinician to run this before sperm selection.
Defective sperm taken into consideration
One factor taken into account during the research was the risk of potentially including defective sperm that wouldn’t naturally achieve fertilisation due to their low motility.
Dr Nosrati says that, like any type of artificial fertilisation that circumvents the fundamental reproductive barriers, sperm that would be naturally discarded due to the lack of motility could be potentially included in the fertilisation process, in turn promoting the transmission of defective genetic traits.
Therefore, future studies on whether IVF fertilisation rates could be improved using sperm samples treated with ultrasound, as well as the genetic testing on the embryos fertilised with sperm treated with ultrasound, are required.
“At the same time, for severe cases of male infertility, particularly for surgically-removed samples from testis, using this method to find a live sperm can add a significant value to current treatment methods,” he says.
The technology has been patented, and the next step will be to run a large-scale clinical trial and pursue commercialisation pathways.
The Monash team hopes to develop partnerships with leading Australian fertility clinics to support the technology’s progress.
“This breakthrough can empower new treatment opportunities to improve the outcome of assisted reproduction, even for couples with severe male infertility that are mostly left with the option of using a donor sample or adoption,” says Dr Nosrati.





