
Some medical breakthroughs involve a single “lightbulb” moment. Others are more like a large jigsaw, where many pieces must fit together before progress can be made.
This was how a group of dedicated researchers developed the FODMAP diet, which is celebrating 20 years of success in helping to ease gastrointestinal symptoms in people with irritable bowel syndrome (IBS).
IBS is a complex condition that historically wasn’t well-managed, lacking any evidence-based therapies that were patient-empowering.
Recognising this, in the early 2000s, a tight-knit Monash University team proposed the FODMAP concept.
The idea built on evidence from numerous studies conducted over many years, showing that the restriction of certain short-chain carbohydrates (lactose, fructose, polyols, fructans and GOS) improved IBS symptoms.
The FODMAP concept was first published in 2005 as part of a hypothesis paper. In this paper, it was proposed that a collective reduction in these poorl-absorbed short-chain carbohydrates would in turn reduce gas and water that can lead to distension of the intestinal wall.This was proposed to reduce stimulation of the gut’s nervous system and provide the best chance of reducing symptom generation in people with IBS.
At the time, there was no collective term for indigestible or slowly-absorbed, short-chain carbohydrates. So, in April, 2005, the team initially led by Professor Peter Gibson, and Dr Sue Shepherd, published the first research paper introducing the idea and naming these carbohydrates FODMAPs.
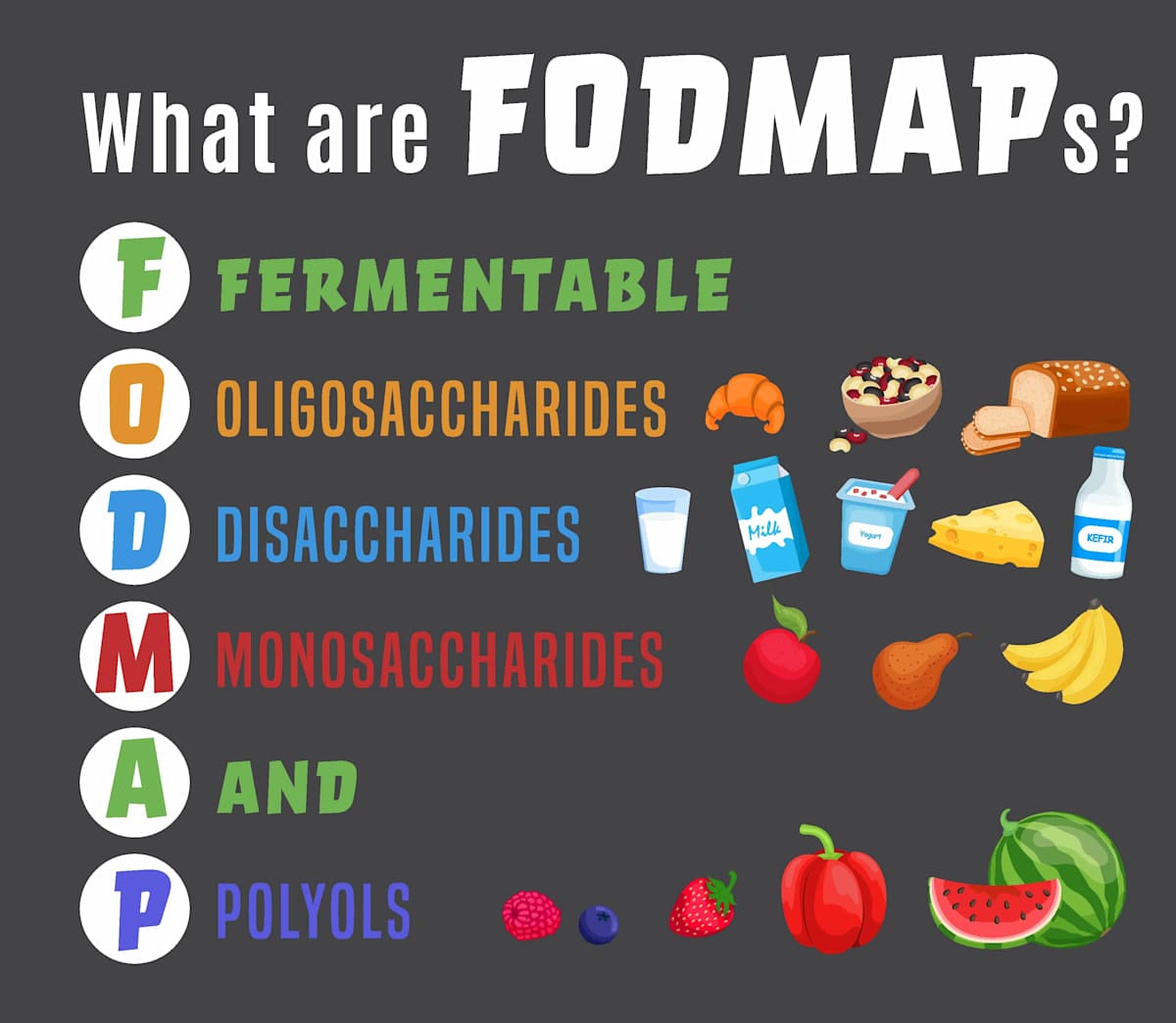
What are FODMAPS?
FODMAP stands for “Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols”, an acronym that aims to improve understanding and facilitate communication of the concept.
Because FODMAPs are found in many foods from different food groups, the team then went on to measure the FODMAP content of a wide range of foods, including fruit, vegetables, breads, cereals, nuts, legumes, dairy products and manufactured foods.
This FODMAP composition data enabled them to develop the low FODMAP diet and conduct studies showing that a low FODMAP diet eases gastrointestinal symptoms for most people living with IBS.
The first of these studies was led by Associate Professor Emma Halmos, and these groundbreaking findings have since been replicated by research groups all over the world, demonstrating that 50-80% of people with IBS respond to a low FODMAP diet.
The team also identified the mechanisms by which FODMAPs trigger IBS symptoms. They found that because FODMAPs are relatively small in size, they attract water into the small intestine.
When FODMAPS reach the large intestine, they’re fermented by resident gut bacteria, producing gas. The additional gas and water inside the gut stretches the bowel wall and triggers IBS symptoms such as abdominal pain, gas and bloating, distension, constipation, and diarrhoea.
The Monash FODMAP app and cookbook
To enable people with IBS to access accurate, reliable information about the FODMAP content of food, in 2012 the team released the Monash FODMAP App.
The app includes thousands of foods laboratory-tested by Monash for FODMAP content and uses a simple traffic light rating system, whereby red foods are high, amber foods are moderate and green foods are low in FODMAPs in a typical serve.
The app, which has been kept affordable with a small one-off fee (now A$12.99) has been downloaded by 1.75 million people in more than 100 countries, and reached No.1 in the medical category in more than 50 countries.
It’s also listed in the American College of Gastroenterology Clinical Practice Guidelines for the treatment of IBS.
Read more: Gut to be good for you: FODMAP cookbook will improve millions of lives
The FODMAP diet should be followed under the guidance of a dietitian in three steps.
In the first step, patients eat mostly low FODMAP foods for two to six weeks. In the second, they complete a series of food challenges to identify which FODMAPs trigger their gastrointestinal symptoms. In the third step, they reintroduce well-tolerated FODMAPs and only restrict a small number of foods containing FODMAPs that trigger their gastrointestinal symptoms.
The idea is to follow a minimally restrictive diet for the long term, striking a balance between good symptom control and adequate expansion of the diet.
Multiple clinical guidelines from countries all over the world now recommend a trial of a FODMAP diet as a first or second-line therapy for the management of IBS.
In 2023, the first Monash low FODMAP diet cookbook was launched. Drawing on years of groundbreaking research, the experienced dietitians used the world’s largest FODMAP database to create 120 recipes, representing cuisines from around the world.
Combining fresh ingredients and pantry staples, Low FODMAP: The Cookbook enables people with IBS to enjoy food that’s delicious and good for them.
Widening the scope
More recently, Monash researchers led by Dr Jane Varney found that a low FODMAP diet could improve gastrointestinal symptoms in women with endometriosis – 60% of women with endometriosis responded to the diet, compared to 26% who responded to a control diet based on Australian Dietary Guidelines.
Throughout, the research team has worked hard to ensure the accuracy of information used.
All this has been life-changing for some, such as Irena in the US:
“As someone who has suffered from IBS for years without much guidance from my [previous] GI specialist, coming across your research and the FODMAP diet has been truly a life-changer. Your app is a great resource and I rely on it multiple times a day.”
And Marissa, from Australia:
“I am a 42-year-old female who has lived with pain and discomfort since I can remember. I have only used the app as a general guide, but the change seemed to happen overnight. I no longer sit at work in pain with the bloating and cramping, and can wear normal clothes again as my stomach is not so blown out and sensitive. I can’t thank you enough. The work you are doing is changing people’s lives.”
It’s gratifying to see this diet improve the lives of millions of people globally, and continue to evolve as we refine and expand our knowledge about FODMAPs.
Training dietitians and patients on how to implement the FODMAP diet was key to successfully translating the science of FODMAPs into practice.
Recognising this, the team developed online courses to teach patients and dietitians how to implement a FODMAP diet for IBS. These courses have been taken by thousands of patients and dietitians from more than 100 countries worldwide.
The team has also translated the Monash FODMAP App into Spanish, Italian, German and French, with Japanese, Norwegian and Dutch translations on the way. It’s a huge task, but worth it to ensure as many people as possible can access the low FODMAP diet.
All of this has been a genuine team effort.
The low FODMAP diet will always be part of Monash University, not particular individuals. However, everyone involved over the past 20 years is rightly proud to have played their part in helping to put diet therapies such as this on the map.
Other individuals and organisations have developed their own apps, diet programs and cookbooks based on the Low FODMAP Diet. To ensure they’re true to the original, visit the Monash FODMAP website, monashfodmap.com/
The Monash University School of Translational Medicine annual public lecture, FODMAPS 20 Years On, is on Tuesday, 16 September, 6-8pm, at the Alfred Innovation and Education Hub, 75 Commercial Road Melbourne. Details here.





