In 2020, while the world was in chaos, a small team of local trailblazers were busily working away in a Melbourne lab to produce Australia’s first mRNA vaccine candidates for a new virus sweeping the globe.
The Monash Institute of Pharmaceutical Sciences (MIPS) team, led by Professor Colin Pouton, had already developed an mRNA platform and were working on a vaccine for influenza before COVID hit. But when China released the genetic data for SARS-CoV-2, they quickly pivoted their research and joined the global race to develop a COVID vaccine.
Backed by both state and federal governments, the vaccine went on to become Australia’s first mRNA vaccine to be manufactured for clinical trials. Since then, results from the Phase 1 clinical trial , conducted in collaboration with the Doherty Institute, have been published in Molecular Therapy Methods and Clinical Development, with the study demonstrating the vaccine’s ability to overcome the COVID-related issue of “immune imprinting” – the process by which exposure to one virus strain, acquired by way of either vaccination or viral infection, starts to limit our immunity against new variants of the virus as they arise.
Not only has Pouton’s mRNA COVID vaccine demonstrated local expertise in the exciting field of mRNA medicines, it also formed the foundation for mRNA Core – a MIPS-based, government-funded initiative comprising a team of scientists working to advance the next generation of mRNA.
More on mRNA Core
Natural mRNAs are a vital part of our regular cellular functions, acting like a genetic barcode that your cells read to reproduce the encoded sequence – typically, a protein or peptide. Scientists can harness this technology for vaccination by designing synthetic mRNAs that encode the sequence for an antigen (a key protein from a virus or other pathogen that can be recognised by our immune system), which our cells can then produce to trigger an immune response without the risks stemming from infection with the real virus.
Because the mRNA “code” can be rapidly written, amended or rewritten, scientists can quickly produce new vaccines or adapt existing ones to take on new viral strains, unlike more traditional protein-based or live-attenuated viral vaccines.
This has made them an attractive option for global virus control methods, and forms the basis for the research and development at mRNA Core.
At any given time, mRNA Core is working with research teams across Australia – and even as far afield as New York – on a vast range of projects, all geared toward finding new preventatives and treatments for a wide range of diseases using mRNA technology.
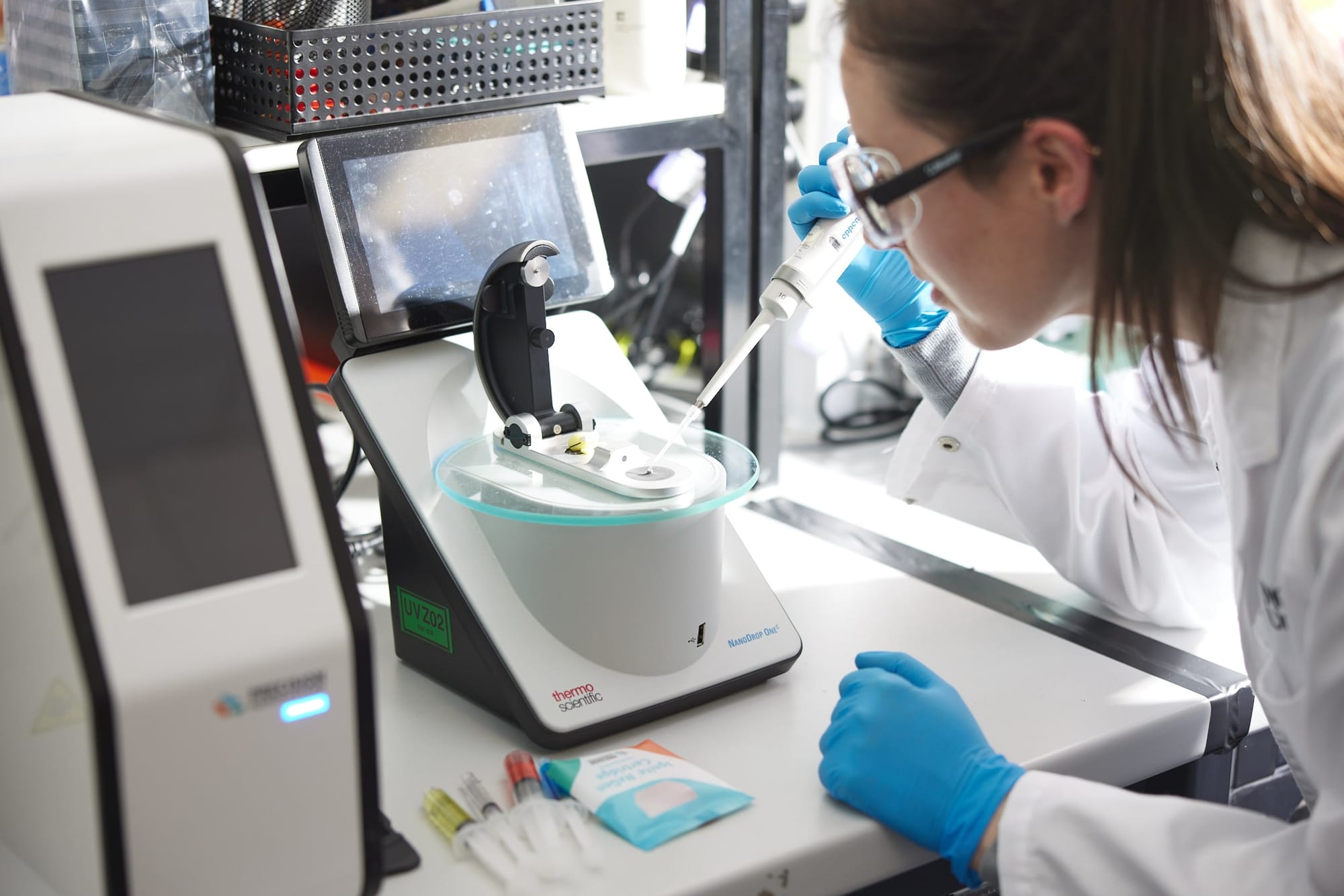
Since its inception, the team has collaborated with research institutes on vaccines and therapeutics for COVID, malaria, fatty liver disease, type 2 diabetes, cancer and tuberculosis. mRNA Core’s central role in these collaborations centres on the design and synthesis of mRNA and mRNA-LNP (lipid nanoparticle) products, which form the basis of a range of therapeutic candidates, from vaccines to gene therapies.
mRNA Core has designed an extensive library of mRNA sequences, through which it’s developed, collectively, more than 600 mRNA-LNP products. LNPs are tiny, spherical particles made of lipids (fatty compounds) used to deliver drugs and nucleic acids. They’re an emerging technology for gene delivery and a key component of mRNA vaccines, as they help protect the mRNA cargo from being broken down or cleared by the body before it can reach the target cell.
Read more: RNA therapeutics: A brave new world expands
In addition to mRNA, RNA products can also include self-amplifying RNA (saRNA), small interfering RNA (siRNA), antisense RNA (asRNA), and microRNA (miRNA). All of these products are currently being explored as RNA therapeutics and vaccines.
Based at MIPS in the heart of the Parkville precinct in Melbourne, mRNA Core is currently funded by a Medical Research Future Fund (MRFF) mRNA Clinical Trials Enabling Grant. The facility is also one of the four national nodes of the RNA Products division of Therapeutic Innovation Australia (TIA), as part of the National Collaborative Research Infrastructure Strategy (NCRIS).

Tackling tuberculosis
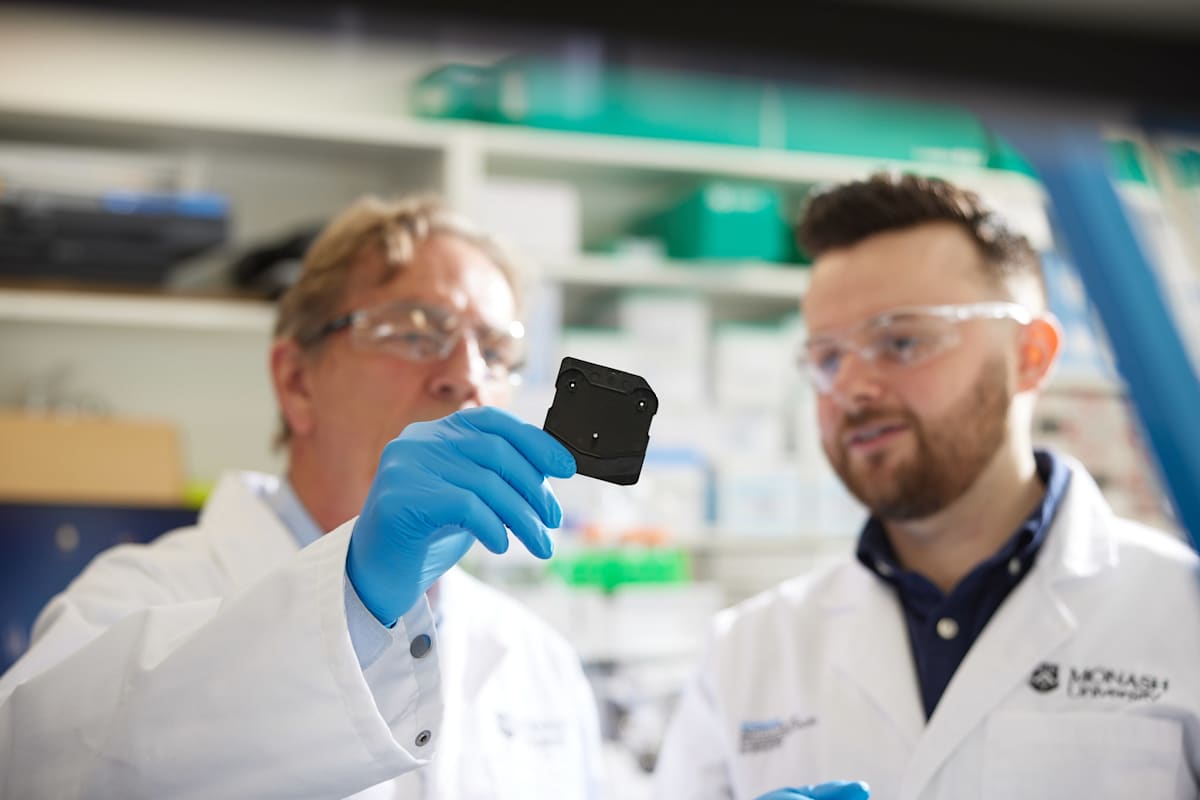
In February this year, a study involving Professor Pouton and his MIPS colleague, Dr Harry Al-Wassiti, was published in eBioMedicine. The study, led by the University of Sydney in collaboration with the Centenary Institute and MIPS, described the development of a novel mRNA-LNP vaccine to boost immunity against tuberculosis (TB) – the largest cause of infectious mortality worldwide.
Currently, the century-old Bacillus Calmette-Guerin (BCG) vaccine is the only approved vaccine for TB, and is used widely despite its effectiveness in adults being inconsistent.
The pioneering pre-clinical trial showed that the mRNA-LNP vaccine effectively triggered a defensive immune response that helped to destroy cells infected with TB. When used as a booster in BCG-vaccinated mice, the vaccine significantly improved long-term protection against TB compared to mice that had received BCG alone.
The MIPS team made key contributions to the tuberculosis vaccine project through developing the mRNA vaccine and its LNP delivery system, redesigning the TB antigen to attract a more robust immune response, and contributing to experimental design.
But the project is a testament to the collaborative spirit of the entire research team, as collective efforts by Australian scientists to advance mRNA technologies continue to establish Australia as a major player in the field of mRNA medicine.
The homegrown TB vaccine represents a major advance in tackling the world’s biggest infectious killer, which is responsible for more than 1.5 million deaths a year, with a particular prevalence in countries such as India, Indonesia, China, the Philippines, and Pakistan.
Given the scale of TB-related deaths and the ongoing urgent need for a new, more effective vaccine to prevent TB, the findings from the eBioMedicine study provide a strong rationale for further clinical development, with the hope that an mRNA-LNP vaccine candidate will ultimately be more effective and consistent than the BCG.

Looking to the future
It’s a challenging time for science, particularly in the field of mRNA and vaccines, where disinformation has been rife. mRNA vaccines and therapeutics still face challenges, in particular the delicacy of the mRNA construct necessitating ultra-cold storage conditions, which limits the ability to provide mRNA medicines to underdeveloped countries and remote or difficult to access areas.
The phenomenon of “immune imprinting” also continues to stymie scientists’ ability to combat emerging strains of existing disease and achieve long-term protection, both through naturally-acquired immunity and responses induced by vaccines, including mRNA technologies.
mRNA Core’s COVID mRNA-LNP vaccine has shown promise in overcoming the challenge of immune imprinting, and scientists at MIPS and around the world are continuously working to overcome these challenges to generate the next generation of mRNA medicines.
Several very exciting and promising products are making their way through clinical trials, including vaccines for influenza, norovirus and cytomegalovirus (CMV).
Further, Moderna and Merck are collaborating on mRNA vaccine candidates against various cancers, in particular head and neck cancer and melanoma, which continue to progress through clinical trials.
Meanwhile at MIPS, mRNA research initiatives have continued to flourish with the recent establishment of the Monash-Moderna Quantitative Pharmacology Accelerator, and Australia’s first National Centre for Biopharmaceutical Optimisation of mRNA Therapeutics (CORTx), which is supported by an MRFF grant, and brings together academia and industry to evaluate mRNA delivery and biodistribution in the body, informing the plausibility of the candidate to progress toward human studies.
This information is critical for maximising the potency, safety, and manufacturability of mRNA medicines.
mRNA Core also continues to thrive with a steady stream of projects flowing through from around the country. Watch this space.





