
Jomo Kigotho is 24 now and back once again in Melbourne, hidden away in the lab most days, making molecules. The young scientist was born in Australia, but spent much of his childhood in Africa at a place that’s still not conclusively on Google Maps, underneath Mount Kenya.
The place – “it’s not a town”, he says, “it doesn’t have a name” – was on a migratory path for elephants coming down out of higher country to the forested national parks and plains below. The Kenyan capital, Nairobi, is nearly five hours away, the equator is 10km to the north. No electricity or running water there when he was a kid.
“It was very, very rural, and sometimes very challenging,” says Jomo’s mother, Ruth Rowlands. “But for some reason the kids thrived. They didn’t seem to take a back step.”
Jomo is the eldest of three; his brother Jamali is also a Monash student, and his sister Malaika is in Year 12 in Tasmania. Their father, Jeff Njuguna, is Kenyan, and from the remote spot in question, around the town of Kitale. While in Australia many years ago he met Ruth, and the couple (now separated) had the kids, then took them all back to his homeland, where they built a school and a home, under the mountain.
The family split their time between Melbourne and Kenya, where the kids were homeschooled. It was their home away from home – but also very much a home – among remote Kenyan wilderness.
Ruth remembers her first-aid kit in the house, stocked with electrolytes. She had a book titled Where There Is No Doctor, the African edition, which came in handy, because at the time the closest medical care was hours away.
“I broke my finger once, but you just sort of manage it yourself,” she says. “Jomo and his brother and sister lived through a lot of stuff.”
The family knew some children and adults with HIV, they knew some orphaned children, they went to funerals. These were the sort of experiences any family might have in a poor, developing country.
Jomo says he was “eight or nine years old” when his experiences among all this started blending with other feelings. What were they? Dreams, ambitions? A fledgling sense of injustice, of right and wrong, of the haves and the have-nots?
“It was a feeling that I would help people, medically, somehow,” he says.

At the heart of research
The lab where Jomo works now is at the Monash Institute of Pharmaceutical Sciences (MIPS) in central Melbourne. He’s a PhD student at the heart of new research into drugs to fight malaria, which, after all this time, is an exclusively “developing world” crisis.
The young scientist is part of a team of nine that’s found a new group of molecules that can kill the malaria parasite. Their research has been published in the prestigious European Journal of Medicinal Chemistry.
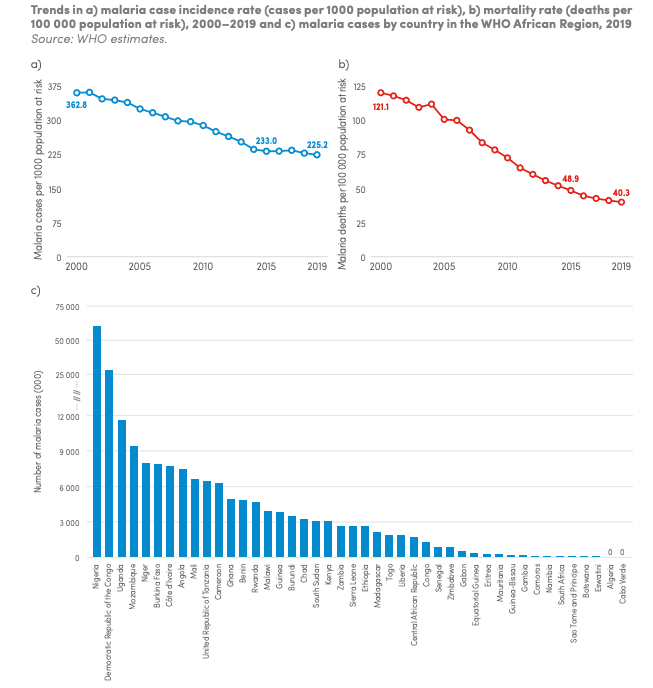
Malaria – caused by parasites in certain types of mosquito – is endemic in Africa, where 90% of all the world’s cases and deaths occur. It kills 400,000 people worldwide a year, with most – nearly 70% in 2019 – aged under five. Pregnant women and those with HIV/AIDS are also at high risk.
In Kenya, death rates in children are actually falling – but it’s still a major public health problem. The majority of the population is at risk of malaria infection.
The problem is, the malaria parasites are becoming increasingly resistant to the current crop of antimalarial drugs. It’s a scientific race to make new treatments that are cheap and effective so that they get to those in poor, remote countries who need them most.
And this where more of Jomo Kigotho’s African backstory comes in.
The family – all five of them – were plagued by malaria regularly in Kenya, despite living at a relatively high altitude, where malaria should be scarce.
Jomo’s younger brother, Jamali, fell ill when he was three, and it was serious; he was delusional with a very high fever in the heart of Africa, the family without transport for those few crucial days to get him to the faraway hospital.
“He got it really bad,” says Ruth. “He was seeing butterflies. It was almost like I had to drip electrolytes into him all night. It’s a scary thing. The fevers are bad, he was so hot; I was laying cool cloths on him, then he’d be freezing, and I’d be rubbing him and rubbing him. It was a horrible thing.”
Little sister Malaika got it badly when she was only six months old. “Little kids can get dehydrated very quickly and die,” says Ruth. “She was unwell.”
Ruth’s had it “a couple” of times, but you sense by “a couple” she might mean five or six. Once, she had malaria and typhoid at the same time, as a mother of three.
Jomo himself has had malaria five times, the worst when he was 17 and had decamped to Kenya for a break after Year 12, and ended up spending 10 days in bed.
He never had it as badly as anyone else in the family, but enough to know how it feels, and enough to see the heartbreak and illness it can cause in malaria-prone communities.
It especially frightened him to see Jamali so sick.
“It’s really bad for kids under five, usually. They die. He was very sick, his head wasn’t there, he wasn’t responsive. He was awake, but I couldn’t talk to him.”
Jamali doesn’t remember what it was like – he was too young – but he knows what he’s been told: “... they said I might have passed away in the night.”
‘It’s terrifying when you look at it closely’
One of the curious things in this story is that Jomo didn’t worry too much about malaria before. It was just a part of life. Plus, he was young, and still learning.
But now that he knows a huge amount about it, both culturally and scientifically, he’s more than worried – he’s scared.
“It’s terrifying,” he says, “when you look at it closely.”
The biggest problem is that the drugs are no longer working.
“I never really knew the extent of drug resistance and how bad it is,” he says. “In Africa and Southeast Asia, the World Health Organisation [WHO] recommends five different anti-malarials, but in Laos three of the five don’t always work, and in Cambodia all five can fail.”
“We need new medicines and new ideas. We need everything – everything – to be worked on.”
In Africa, new resistance to one of the primary drugs was spotted last year.
“It’s a terrifying thought that you or I could get malaria, and the medicine doesn’t work,” he says. “But that’s where we’re at.”
One of the key questions in mosquito and malaria control is: What’s better – kill the actual mosquitoes in the wild, or kill the parasite from the mosquito?
All through malaria-prone countries, the streets and towns are sprayed with insecticide regularly, to kill.
In Indonesia, a new trial by the Monash-aligned World Mosquito Program infected trial mosquitoes with a bacteria called Wolbachia. Researchers found the bacteria stopped the mozzies hosting the dengue virus, so they released the bugs into the city of Yogyakarta, which has seven million dengue cases a year, a huge public health burden. In two years, cases requiring hospitalisation dropped 86%.
Similar trials have been carried out in Brazil and Colombia for Zika, a malaria-like, mosquito-borne illness that’s similarly dangerous for babies and children, but can also cause the rare paralysing condition called Guillain-Barré Syndrome (GBS).
“There are many tactics,” says Jomo. “The Indonesian work is very clever, but very hard to do. What we’re working on is an actual medicine to give to people when they get malaria.
“One of the things that has helped malaria in Africa this century is getting mosquito nets out to where the kids are sleeping. But there are always cracks in the system, and we need medicines to turn to.”
He’s a passionate advocate for equality in healthcare, as well as the hardcore science behind trying to make new drugs.
“We need new medicines and new ideas. We need everything – everything – to be worked on.”
At the Monash University lab, the molecules the researchers have discovered contain a chemical compound, a phenol, that’s potent against the parasite. The molecules (atoms, joined together) are the 2-aminobenzimidazoles, or ABIs.
Study co-leader and Jomo’s supervisor, Dr Shane Devine, says the discovery is scientifically exciting because of the pure chemistry involved, but also because of growing resistance to current drugs.
“Through a number of chemical modifications, our team has been able to alter the molecules so that it can kill the malaria parasites more effectively, with the most potent molecule representing a remarkable twelve-fold gain in antimalarial activity from the starting molecule.”
The molecule ticks all the boxes so far – low molecular weight, high efficiency, highly soluble, and easy to manufacture. It works through a new mechanism to which the parasite hasn’t been able to generate resistance.
“Our molecule is exciting because it’s relatively easy to access,” Jomo says. “So it should be cheap to make as a drug. You need to make these molecules at a low price in developing countries, so this is good. Other research I’ve seen is very complex and therefore will cost more at the end.”
Jomo has had malaria five times, the worst when he was 17 and had decamped to Kenya for a break after Year 12, and ended up spending 10 days in bed.
Consider also, knowing that such breakthroughs are only now emerging, that malaria is an ancient disease – historians have found references to something much like it from the 6th century BC, in China.
For thousands of years the disease was unnamed, and assumed to come from a local rotting “miasma” of dead animals, old food or swamps. There’s a theory that the word malaria comes from the Italian mal’aria, meaning “spoiled air”.
Old medicine also had plagues, cholera, and many other misfortunes coming from the “miasma”, the ether. They had no idea what it was, except that it killed people or made them very sick.

As outlined here by Professor Francis Cox, a former dean of science at the University of London, parasites in the blood of malaria patients were first found in 1880; the science of how the parasites breed in 1897; and that malaria is given to humans by mosquitoes in 1898. The fact that it makes a home in the human liver wasn’t discovered until after WWII.
Only the female of one of 40 types of an Anopheles mozzie can transmit it, and they must have been already infected through a previous blood meal from an infected person. It’s a sneaky, nasty disease made sneakier and nastier because it comes from tiny flying insects.
The reason this sub-set of female mosquitoes bite us in the first place is because human blood helps them produce their own eggs.
The parasite is only single-cell, a tiny micro-organism, or “protozoan”. It basically pollutes the red blood cells, then breeds in the liver, causing, at best, fever and nausea, and at worst, death.
“It’s a terrifying thought that you or I could get malaria, and the medicine doesn’t work. But that’s where we’re at.”
Because it’s in the blood, it can be transmitted by anything carrying blood – transfusion, syringes, transplant, and in or from the womb. The mosquitoes themselves are immune to the disease they carry, a quirk that may unlock more scientific discoveries and potential drugs.
The higher the rate of community disadvantage where the mosquitoes bite people, the worse things will be – poor, remote places with little healthcare and unclean water will always suffer.
Malaria is now resistant,at least partly, in some geographic locations, to chloroquine, sulfadoxine/pyrimethamine, mefloquine, halofantrine, quinine, and also artemisinin-based combination therapies, which are the go-to drugs all over the world.
“It’s a problem for all of us if the resistant parasites become more widespread,” says Jomo.
One difficult irony here is that two of the most effective malaria drugs for a very long time – quinine and artemisinin – were made from ancient natural remedies, a tree bark and a woody herb, but the lifespan of medicines from the bark and the herb appears to be coming to an end.
A legacy built in Kenya
Jomo Kigotho did his first year of high school in Kenya, homeschooled with Australian textbooks by Ruth, his mother. Then they moved to Tasmania to the small town of Ulverstone, on the northern coast near Devonport, where Ruth’s from.
The school the family set up back in Kenya grew from just a handful of students to 700. It’s run by others now that Jomo’s mother and father aren’t together, but it’s thriving.
“It was a shame to lose it,” says Jomo, “but my parents had a good 15 to 20 years of progressively growing it. A lot of the kids wouldn’t have gone to school otherwise.”
One of the initiatives there was to give young teenage girls philanthropic-funded scholarships to attend the school, because once they were in arranged marriages, they didn’t go.
They also dug a bore to avoid dirty water, and built water tanks to get more kids into school instead of their usual job of collecting water. They set up a care program for orphans, another for single mums, and a women’s group. They also bought a mill for maize.
The work of Jomo’s parents had attracted significant attention. Ruth met a pre-presidential Barack and Michelle Obama in Chicago through a wealthy Democrat philanthropist who backed them – the Obamas were set to visit the Kenyan site while he was campaigning, but due to the remoteness, the trip was called off for security reasons.
“That’s another story,” says Ruth. “We do have a few.”

The brothers began refining their views on social justice and economic inequality. They also egged each other on as high school drew to a close, both aiming for the highest VCE scores they could.
Jamali is now at Monash University studying engineering and science, majoring in mechanical engineering and physics.
“One thing Jomo likes to constantly bring up,” says Jamali, “is even though I’m studying physics, he beat me in physics in Year 12. He loves to bring that up.
“We had a bit of a running bet about who got the highest ATAR, and I was lucky enough to win that one, but he holds onto beating me at physics, which is now my degree. But I hold it to him that I beat him at organic chemistry, which is what he went into. Just a good bit of brotherly competition.”
Jamali’s interested in renewable power generation, and has been involved in University and private projects, including designing a net zero domestic violence refuge – “to show that solar and renewables can help solve social issues”, he says.
He’s also designed a small power station with the aim of enabling Kenyan and pan-African children more access to laptops.
“Education is the biggest issue in Africa,” he says. “People don’t necessarily like relying on charities. They say, ‘Give us an education so we can solve our own problems’.”
Read more: From Baghdad to Melbourne: Dr Harry Al-Wassiti's remarkable journey
He says his older brother is, well, a bit of a legend.
“Jomo is one of the smartest people I’ve ever met. He doesn’t take himself too seriously, either, especially outside of work. He’s very relaxed; no one dislikes him. He loves sport – he could talk about sport for days.
“He loves learning. I was talking to him recently, and he said he’s reading four or five books at the same time. He’s into the histories of cultures people don’t know much about. He has multiple daily news podcasts he listens to.
“It’s like he was born an adult. Even as little kids, he always wanted to be at the adults’ table and discuss things with them, serious topics. He was always fun, but he also always enjoyed knowing things, and trying to use that to help people.”
At Monash, Dr Devine first met Jomo when the budding young scientist was in his second undergraduate year.
By that stage Jomo had survived his “very rough” first year after moving to Melbourne from Tasmania. He was house-sitting for a family friend in Broadmeadows with a scholarship and interstate-student allowances, but limited income support beyond that, and only a small network of friends.
“At one stage in my first semester I had 40 cents to my name,” he says. “My parents are mad at me now, because they didn’t know I was struggling. But my mindset was, ‘I am going to uni, and I am going to get myself by’.”
Only a ‘neglected’ disease in the developed world
In his third year, he joined a pharmaceutical sciences lab project on malaria, and found his calling.
One of the key reasons why this is: Malaria is called a “neglected” disease in developed-world countries such as Australia, which has no malaria. For someone from one of the 100 countries where it’s still found – in Africa, Asia, Central and South America, the Caribbean, the Middle East and the Pacific – “neglected” isn’t the way malaria’s talked about.
Australia’s Northern Territory and north Queensland – and islands in the Torres Strait – have the mosquitoes that can carry malaria, but are essentially malari-free because it’s been bred out by easy access to antimalarial drugs (which most can afford), the chemical DDT (until it was banned), and costly government projects such as draining swamps and housing tracts.
This is where Jomo’s passion comes from, having seen both sides, and having seen that one side always wins and the other side always loses. He thinks that’s what makes him a good scientist, too.
“I like to think so,” he says. “I like to think it helps that I’ve a good understanding of what we are trying to fix. I’ve seen it. I’ve been to funerals of people who have died of malaria, and as someone who has a connection, it gives me a good understanding of how important this is.”





