High cholesterol levels from birth can be caused by a common genetic condition called familial hypercholesterolemia (FH). It can lead to a high risk of coronary heart disease from an early age, and some estimates suggest that by the age of 70, one in every two patients with FH would have had a coronary heart disease event.
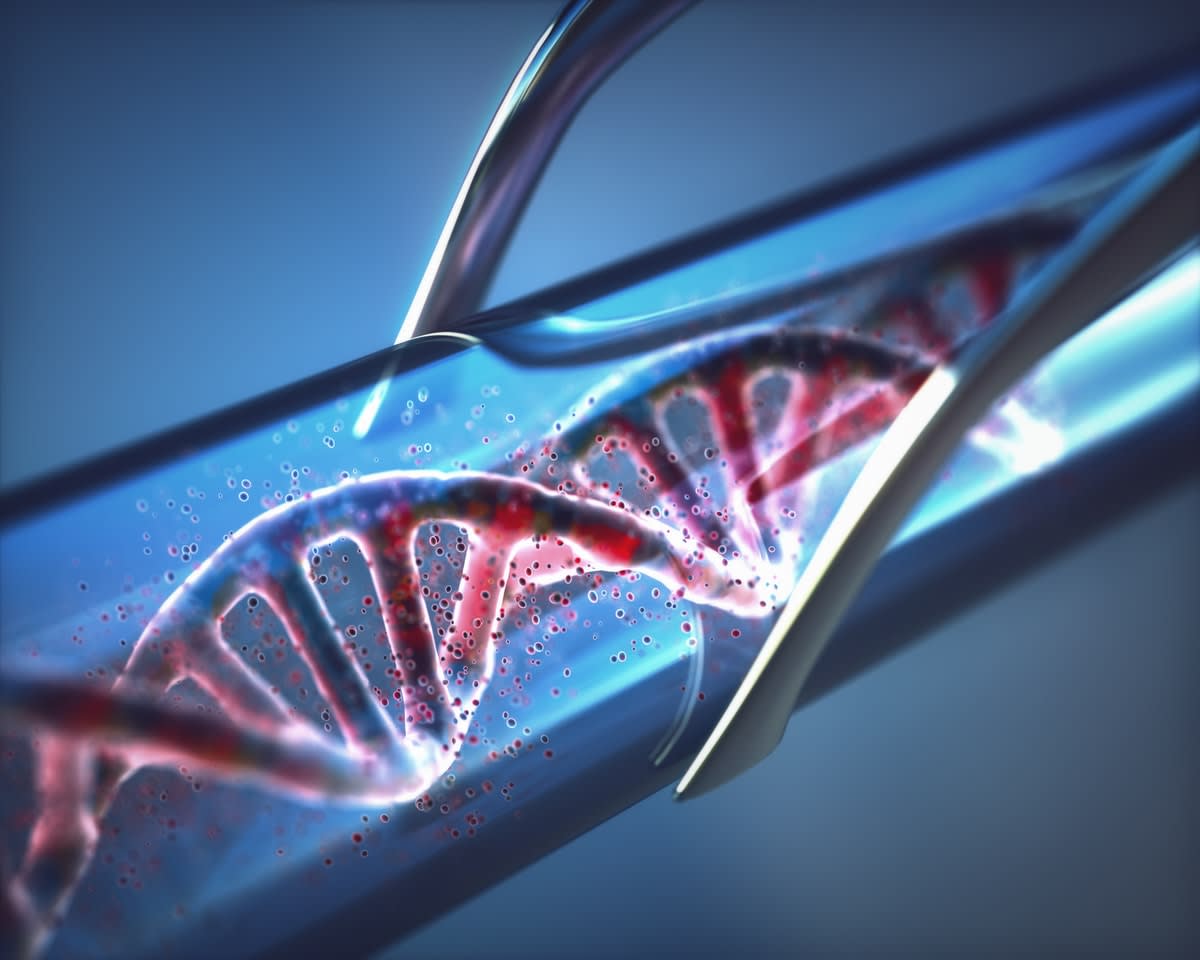
The good news is that the increased risk of coronary heart disease for FH patients can be managed and reduced with lifestyle modifications and lipid-lowering medications that are effective and generally safe. Also, people with FH can be identified with precision using a single DNA test.
The less-than-good news is, however, that few Australians have access to this DNA testing to detect their risk of FH.
More than 30,000 people in Australia are living with FH, but estimates show only 5-10% are being diagnosed.
Identifying these individuals and lowering their cholesterol levels is vital to lowering their risk of suffering from premature coronary heart disease, which can be fatal.
Limited testing part of a missed opportunity
This missed opportunity for diagnosis is likely due to many factors, but a large part, we believe, could be due to limited access to DNA testing currently offered through the Australian public healthcare system.
The strict eligibility criteria set for DNA testing means only a small number of people meet the conditions for testing, leaving the majority of the FH population undiagnosed and untreated.
Read more: Matters of the heart: Tackling a disease that kills one Australian every 12 minutes
Our position is that offering universal access (that is, testing everyone in a population) to DNA testing for FH in early adulthood via the public healthcare system could identify thousands more people with FH early, who could then be provided access to prevention that would save lives. Our ideas are outlined in this new paper in the European Heart Journal.
This strategy could be cost-effective for the health system and society as a whole, since it will decrease the medical costs of treatment and management of established coronary heart disease, and potentially less loss of productivity.
Using demographic data from Australia, and published data from these main cohort studies from FH patients, we built a mathematical model that estimates coronary heart disease and premature death for everyone living with FH in Australia. The model was validated by cardiologists and epidemiologists to ensure all the assumptions made were accurate and represent the nature of the disease with as much precision as possible.
The more patients we are able to detect and treat, the lower the risk of coronary heart disease.
In order to not overestimate the gains from population genetic screening, we set the detection rate of FH in the current situation at 10% (although it could be much lower than that) using data from Australian-specific studies.
In our base-case results (that is, the main analysis), we set the detection rate of population genetic screening at 100%, since potentially all FH patients could be diagnosed with this strategy.
Model tested in eight countries
To gain an idea of how this strategy could work in other high-income countries like Australia, we adapted the costs considering the differences in health services use and healthcare prices between the different settings. We tested the model in another eight countries.
Our model estimated that 33,191 individuals currently have FH in Australia, with the vast majority of them undiagnosed and untreated. Over the lifetime of the population (that is, if we follow up everyone alive today until they die), the model estimated that implementing genetic screening to detect and treat FH patients will prevent 3093 CHD events, including 1279 coronary heart disease-related deaths.
These gains in health will result in a gain of 33,488 years of life lived, and 51,790 quality-adjusted life years (QALYs).
With all the health gains, population genetic screening for FH would be cost-effective from a healthcare system perspective if the cost per test was lower than A$250, yielding an incremental cost-effectiveness ratio lower than A$28,000 per quality-adjusted life year gained.

Cost-saving in every setting
From a societal perspective (considering productivity losses), population genetic screening could be cost-saving, meaning the reduction in productivity losses will completely offset the costs of testing the entire population. The results in other countries yielded similar conclusions, with the societal perspective being cost-saving in every tested setting.
For healthcare systems to be sustainable, we need to find strategies to maximise health while allocating resources in the most effective way.
Cardiovascular disease, in particular FH, represents an unaddressed burden in terms of loss of health and increased cost. These results provide an important foundation to help tackle the unaddressed burden of FH using strategies and tools available right now.