As we approach the World Health Organisation’s (WHO) target to eliminate viral hepatitis in 2030, there’s an urgency to unify efforts across governments, healthcare providers and communities to transform how it is perceived, diagnosed and treated. Despite remarkable global progress, the burden of this disease remains high, especially in Southeast Asia.
World Hepatitis Day, observed annually on 28 July, serves as a reminder of the importance of global awareness, solidarity and renewed commitment to the elimination of viral hepatitis.
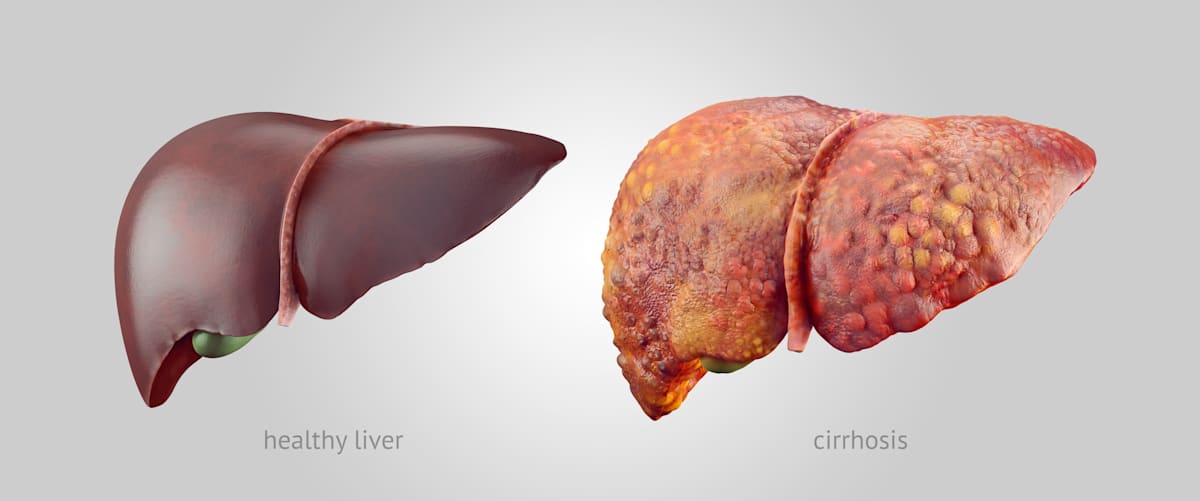
It’s estimated that 354 million people worldwide are living with chronic hepatitis B or C, and more than 1.1 million die each year from complications such as liver cirrhosis and hepatocellular carcinoma.
Due to the silent nature of the disease, millions live asymptomatic, undiagnosed and untreated, and unknowingly spread the infection within their community.
The regional and national burden in Southeast Asia
The WHO Southeast Asia Region (SEAR) considers hepatitis B and C to be a major public health challenge, with an estimate of more than 60 million people living with chronic hepatitis B and C combined. Countries such as Indonesia, Thailand, Myanmar and Vietnam continue to report high prevalence rates.
In Malaysia, hepatitis B affects approximately 5% of the adult population, while hepatitis C prevalence is estimated at 1.9%.
However, this figure is believed to be underreported due to low testing rates, particularly among the highly vulnerable groups such as incarcerated individuals, people who inject drugs, HIV coinfection patients and rural populations.
The major challenges to reducing the burden of viral hepatitis in Malaysia are underdiagnosis and undertreatment.
Barriers to detection and treatment
There are multiple challenges that exist despite the major advances in hepatitis management. The main barriers are:
- Lack of public awareness about viral hepatitis, including risk factors and modes of transmission. Most individuals with chronic hepatitis are unaware of their status until significant liver damage has occurred due to the asymptomatic nature of early infection.
- Limited knowledge among healthcare professionals regarding hepatitis diagnosis and management.
- Inaccessible testing and limited routine screening. Many health systems do not incorporate hepatitis testing into standard health check-ups.
- Stigma and discrimination. There are misconceptions regarding transmission, and high-risk groups discourage individuals from seeking medical care.
- Out-of-pocket costs and financial constraints continue to limit access to antiviral therapy for hepatitis B and direct-acting antivirals (DAAs) for hepatitis C.
Innovations in diagnostics and surveillance
To reduce the burden of hepatitis, innovative and affordable approaches to testing and monitoring treatment response are essential.
Encouragingly, advances in diagnostic technologies and surveillance systems are beginning to transform the landscape of hepatitis care, and include:
- Point-of-care testing, including rapid diagnostic tests (RDTs) for hepatitis B and C, enables community-based screening within minutes.
- Dried blood spot (DBS) testing offers a low-cost, easily transportable sample option for remote and rural areas.
- Reflex testing algorithms, where positive antibody results automatically trigger confirmatory and genotyping nucleic acid testing, which reduces the delay in diagnosis and treatment initiation.
- Digital dashboards for real-time surveillance help health authorities identify hotspots, track treatment uptake and plan targeted interventions more effectively.
- Cross-border surveillance and information-sharing through ASEAN health platforms enhance disease mapping and outbreak response.
Malaysia’s public health policy that makes a difference
Malaysia has officially committed to the WHO global health sector strategy and made commendable strides by decentralising hepatitis services and introducing cost-effective treatment options.
As a WHO member, Malaysia is committed to the following goals between 2016 and 2030:
- A 90% reduction in new hepatitis B and C infections
- A 65% reduction in hepatitis-related deaths
- 80% of eligible individuals receiving treatment
In 2017, Malaysia became one of the first countries in the region to issue a government-use licence for sofosbuvir, paving the way for affordable access to generic DAAs for hepatitis C. As a result, hepatitis C treatment became available at more than 50 public health clinics nationwide, improving access for the underserved population.
Another achievement includes the integration of hepatitis B and C screening into HIV, TB and drug rehabilitation clinics, which has increased testing coverage and co-management of these diseases.
Universal hepatitis B vaccination
Malaysia introduced universal hepatitis B vaccination in 1989. Today, the infant vaccination coverage exceeds 95% for the complete three-dose schedule.
Special attention has been given to increasing birth-dose vaccination within the first 24 hours of life, particularly in rural and underserved populations. This step is critical in preventing mother-to-child transmission, which accounts for a significant proportion of chronic hepatitis B cases.
Since the introduction of universal hepatitis B vaccination, the incidence among children under five has dropped to fewer than one case per 100,000 annually, meeting the WHO target.
Harm reduction and prevention policies
To prevent new infections, Malaysia has expanded harm reduction services, including needle and syringe exchange programs and opioid substitution therapy. These services aim to reduce hepatitis C transmission among people who inject drugs, a key driver of the epidemic in the region.
National policies have also established strict measures to ensure the safety of blood products. All donated blood undergoes mandatory screening for HIV, HBV, HCV and syphilis, and regular blood donors receive HBV vaccination free of charge.
Expanding screening and diagnosis programs
Malaysia’s national strategy emphasises expanding hepatitis screening among both high-risk groups and the general population. Target groups include:
- pregnant women
- blood donors
- people who inject drugs (PWID)
- prisoners
- healthcare workers
Community-based screening initiatives, often in collaboration with NGOs and academic institutions, have been introduced to reach broader segments of the population.
Innovative access to hepatitis C treatment
Malaysia made international headlines by pioneering affordable access to hepatitis C treatment through generic direct-acting antivirals (DAAs). In collaboration with the Drugs for Neglected Diseases initiative (DNDi), Malaysia introduced locally-produced medicines sofosbuvir and daclatasvir, breaking barriers to treatment access.
This approach has enabled thousands of Malaysians to receive curative treatment (95-98%) at significantly reduced costs, setting a regional example for other middle-income countries.
National strategic plan for hepatitis
Malaysia has formalised its efforts through the National Strategic Plan for hepatitis B and C. Coordinated leadership drives progress, including the development of a National Hepatitis Action Plan aligned with WHO elimination targets, and monitoring and evaluation frameworks supported by national hepatitis registries and surveillance systems.
Public awareness and community engagement
A significant challenge in hepatitis elimination is overcoming public stigma and lack of awareness. Malaysia addresses this through national campaigns tied to World Hepatitis Day and ongoing educational outreach efforts.
Collaboration with patient support groups and civil society organisations helps bridge gaps in community engagement.
Hepatitis elimination is a shared responsibility for a healthier future. It demands coordinated action across sectors and society. Research institutions and universities must continue generating data on local epidemiology, treatment outcomes, and barriers to care, especially among vulnerable populations.
In Malaysia, academic partnerships have been vital in evaluating decentralised treatment models and optimising screening strategies.
Multi-sectoral collaboration is key. Governments, NGOs, private industry, and civil society must align on a national hepatitis plan that includes targeted outreach, budget allocation, and policy reform.
The engagement of the Malaysian Ministry of Health, pharmaceutical partners and community-based organisations has proven that effective public-private models are not only possible but powerful.
Most critically, community engagement must be the heart of our strategy. By educating the public, training frontline workers and empowering patients, we can dismantle stigma and bring testing and treatment to where people live.





