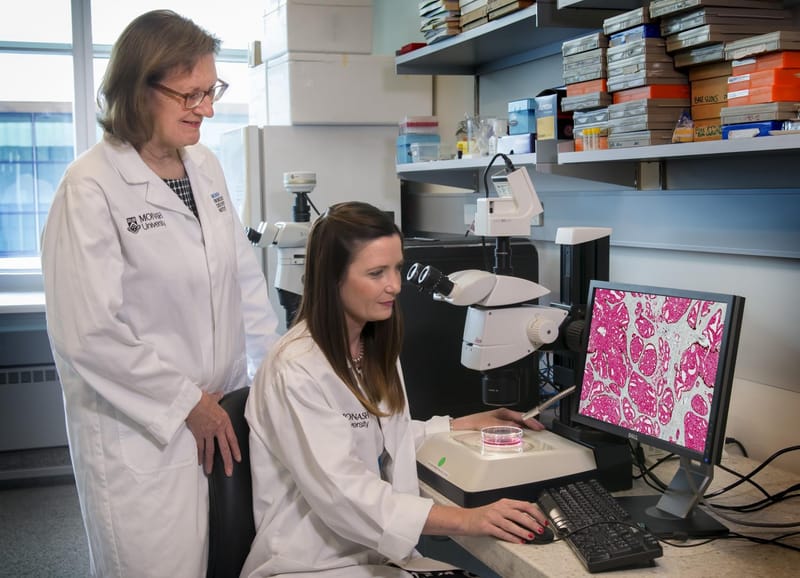
Monash University’s Professor Amanda Thrift has been studying health in rural, impoverished southern India since 2004. Her main interests are hypertension (high blood pressure) and stroke.
Now, as part of an international team, her findings have been published in prestigious medical journal The Lancet, and it’s not a pretty picture. But it does come with a set of recommendations to halt what she calls a pending “huge epidemic”.
The paper, Prevention of stroke: a global perspective, is a review of the methods that could be used to reduce the risk of stroke. It hones in on the contrast between high-income countries and low to middle-income countries. It draws on some findings from 2013’s Global Burden of Disease study, by the University of Washington’s Institute of Health Metrics and Evaluation, and 2017’s INTERSTROKE project, by Canada’s Population and Health Institute.
Professor Thrift is one of nine contributors. She says most of the risk factors for stroke are modifiable, but low to middle-income countries are highly vulnerable. “It’s likely there’ll be a huge epidemic unless something is done.”
A growing gap between high and low-income countries
The numbers are stark, according to the Prevention of stroke paper. There are about 10 million new strokes globally per year. The gap between high-income countries and low to middle-income countries is growing, with approximately 75 per cent of stroke deaths and more than 80 per cent of disability-adjusted life years (DALY) occurring in low to middle-income countries. Stroke accounts for 113 million DALY’s per year, globally. One DALY can be equated to one lost year of a “healthy” life, according to the World Health Organisation.
The key figure cited in the paper is this: in low to middle-income countries there’s been a 100 per cent increase in strokes in 40 years, while in high-income countries it’s decreased by 42 per cent. Professor Thrift says this disparity is “huge” and was a surprise to her.
Low to middle-income countries in Asia and the Pacific, according to the World Bank, include India, Indonesia, PNG, the Solomon Islands, Thailand, Vietnam and the Philippines. Australia is a high-income country.
In India, which Professor Thrift knows best, the reasons are many. The first is cigarettes. The tobacco companies have targeted countries such as India, where legal restrictions around sales, advertising and marketing are looser.

She says economic development in India has changed diet and lifestyle, and led to more sedentary lifestyles. “When I first went to India 35 years ago, I remember Delhi particularly, it was rare to see an overweight person, let alone an obese person, but now,” she says, “they’re everywhere.” Even factors such as modes of transport have made a difference – fewer people in India walk and more ride scooters or drive cars.
Salty issue
Then there’s salt. In 1930, activist Mohandas Ghandi led the Salt March, a 26-day peaceful protest walk against new British taxes and the blanket ban on Indian-made salt.
All over the country, as an act of civil disobedience in support, Indians broke the colonial laws by continuing to make salt or buying black market salt, leading to outbreaks of violence between soldiers and citizens, and several hundred deaths of non-violent protestors in a massacre. So salt, which can contribute to high blood pressure, is not only a heavily-used food flavouring in India, but a cultural and political symbol engrained into the national psyche.

The paper reveals that modifiable risk factors, or things that people can change such as smoking and diet, account for 90 per cent of the global burden of stroke. Dietary factors include not enough vegetables and fruit, and too much salt and sugar – especially in sweetened drinks.
The paper’s authors outlined preventative measures that can be used to quickly and effectively reduce the risk of stroke. They include increasing the price of tobacco, using more mass-media anti-smoking campaigns and passing smoke-free laws, more bands of tobacco advertising, sponsorship and marketing, and cigarette warning labels. In what are described as “strategies to end the tobacco epidemic”, the authors suggest raising the legal smoking age to 25 and banning the sale of cigarettes to people born in a certain year to create what they call a “tobacco-free generation”.
“It’s about trying to find the cheapest options that can be implemented relatively quickly country by country,” Professor Thrift says. “Some countries have already made great gains – for example, in India they have 80 per cent of the front of cigarette packets covered in pictures similar to what we have here. These type of strategies have an impact in changing behaviours and reducing people’s risk of stroke or cardio-vascular diseases.”
Sugar tax recommended
The authors also support taxing sugary drinks. In Mexico, a 10 per cent tax led to a six per cent decrease in sales. They also support “healthy cities” that encourage walking and cycling, “polypills” aimed at people with more than one risk factor for stroke, and more education programs on hidden salts in common foods.
Professor Thrift says in low to middle-income countries such as India, the healthcare community is more geared towards infectious diseases than prevention, and that doctors in rural or remote areas were often overwhelmed by the sheer number of people to look after.
She said “task-shifting” and “mHealth” can help. Task shifting involves taking some tasks away from doctors and giving them to healthcare workers; it’s been shown to be effective in hypertension contexts. mHealth is the use of mobile phone apps.
“These apps can give the healthcare workers more knowledge and help them follow recommended procedures,” she said. “It also enables the local doctors to see test results, such as blood pressure measurements, in real time. Then they can act if need be.”