About 1.5 per cent of the female population worldwide has endometriosis. It’s a chronic disease formed by tissue such as the lining of the uterus (the endometrium). This tissue forms lesions that stick on, and sometimes invade, organs such as the ovaries and bowel.
Endometriosis is finally a hot topic.
We’re hearing more and more women’s stories of having their pain dismissed by loved ones and doctors. Stories of lives being derailed by debilitating symptoms caused by endo. And stories of strength and determination to make the next woman’s experience a little better.
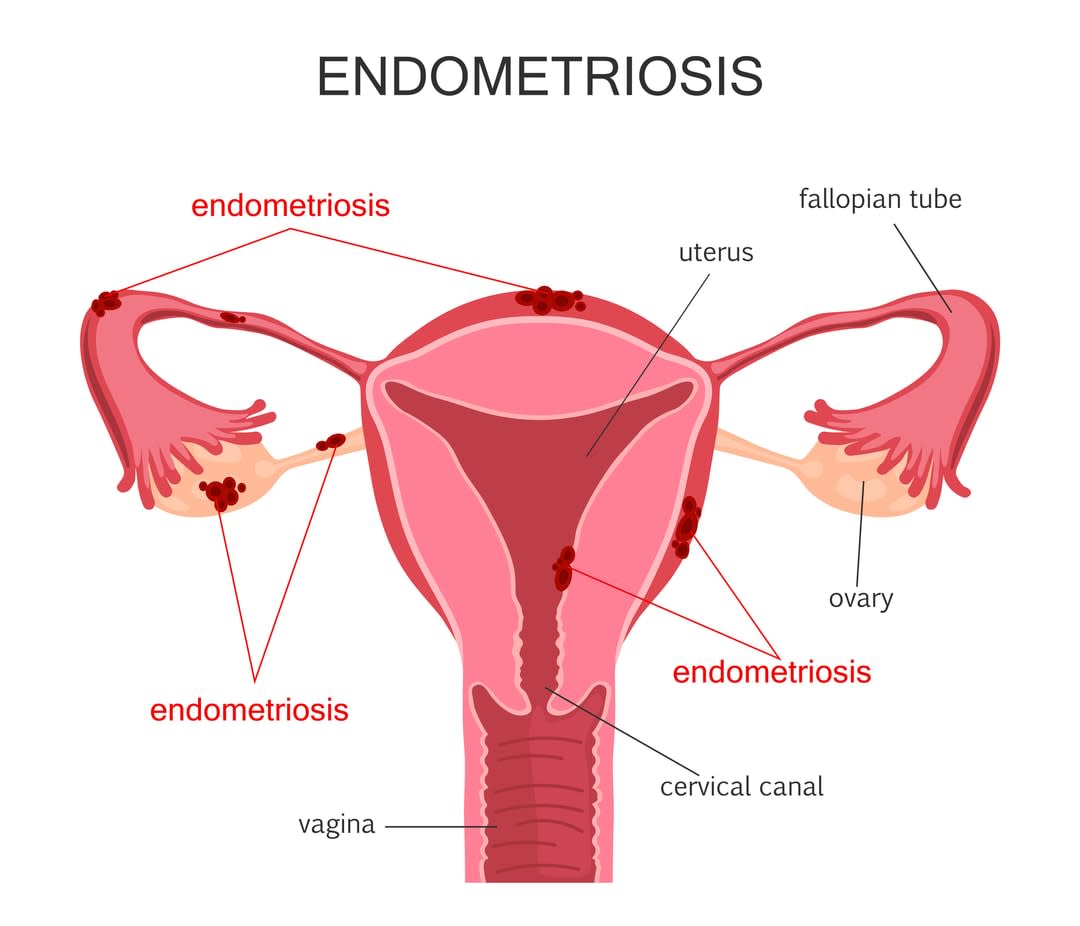
Symptoms of endometriosis include painful and heavy periods, diarrhoea and painful sexual intercourse, to name a few. The most accurate form of diagnosis is through surgery. The disease can be removed by surgery and managed with hormonal therapies (such as the contraceptive pill), though about half of all women will redevelop symptoms after treatment.
As a public health researcher, I’m interested in how healthcare for endometriosis can improve women’s experiences of the disease and lives overall.
My research addresses the social, cultural and historical factors that shape what goes on between women and their doctors. Are these interactions meeting women’s diverse needs? And does their healthcare foster their full participation in society?
Improving care for women with endometriosis
My research with doctors suggests there’s room for improvement.
I interviewed eight gynaecologists and four GPs about their views on providing care to women with endometriosis.
The doctors expressed empathy and concern for women with endometriosis. However, they were challenged by those they didn’t know how to help. (This is a lot of patients, considering there’s no effective long-term treatment for at least half of all women.) In response to this challenge, clinicians often turned to the ‘hysteria myth’.
Related: Does anyone have a pad? TV is finally dismantling the period taboo
The hysteria myth attributes the cause of women’s illnesses – usually ones that have no clear medical explanation at the time – to their psyche (mind) and failure to uphold their ‘biologically destined’ role of mother. An example of this is Plato’s wandering womb – disease in women was attributed to their uterus wandering around their body, with the ‘cure’ being pregnancy to anchor it. This is echoed in the modern-day trend of doctors recommending pregnancy to women with endometriosis, despite no research evidence for benefit.
There’s little quality research to guide doctors in their care of women with endometriosis. They’re expected to always have an answer for the people who seek their care.
Most doctors began their interview by distinguishing between what we termed ‘good’ and ‘difficult’ patients (labelled by one gynaecologist, the “endometriotic cripple”).
- ‘Good’ patients were women who accepted their doctor’s interpretation of their disease and symptoms, and didn’t pose a challenge to their doctor.
- ‘Difficult’ patients were typically women who didn’t find relief from available treatments and who repeatedly returned for help. These women’s symptoms were attributed to their psyche. As one gynaecologist said:
“They [women] make that the focus of a lot of things that go wrong, and perhaps endometriosis has to play a larger part in their lives than it necessarily has … Depending on their … psychological system and ability, I think they make that the focus of their lives, the reason why they can’t go on and do things. They’ve got something to blame.”

Another gynaecologist, however, made a similar distinction but with no value judgement. She said:
“Some people are able to be philosophical about those kinds of things and think, ‘Oh, you know, that’s what nature’s dealt me and I’m just going to have to deal with it and get on with it.’ And for other people it’s a grief response that is much more difficult to deal with and find their way through, and the extent to which that’s influenced by things like people’s sense of self-worth that might relate to their employment or other roles in life … There’s a whole lot of things; I don’t think it’s simple.”
When asked about the potential impact of living with endometriosis on women’s mental health, one gynaecologist stated: “Do mad people get endo or does endo make you mad? It’s probably a bit of both.” Another hypothesised that one of his patient’s symptoms was a “psychosomatic expression” of “matrimonial disharmony”.
Women deserve better
As a woman and feminist, these things were hard to hear. But they weren’t surprising. These findings are consistent with the research into women’s experiences of endometriosis and with the stories shared in the press and social media. There’s no question that women deserve better than this.
But the answer doesn’t lie in condemning individual doctors.
Doctors attributing women’s symptoms to their psyche reflects society-wide beliefs about women and their bodies that have persisted for much of documented human history. (Remembering that it’s largely men who have been doing the documenting.) Beliefs that the sole purpose of women is to reproduce, that they are volatile and controlled only by their raging hormones, and that they’re not to be trusted or believed. These are beliefs that we all, including myself, participate in perpetuating to varying extents.
There’s little quality research to guide doctors in their care of women with endometriosis. They’re expected to always have an answer for the people who seek their care. Our medical system and culture make it difficult for a doctor to say, “I’m sorry, but I don’t know how to help you.” (Though the women in my research valued doctors who did do this.)
We must give clinicians the training and support they need to provide comprehensive healthcare for women with endometriosis. This care should foster women’s full social and economic participation; clinicians need the skills to recognise when their practice may be impeding it.
We must do better.