One day three years ago, Dr Fernando Gordillo Altamirano was beavering away in a Monash University microbiology lab trying to figure out a link between the worst antibiotic-resistant hospital superbug of them all, Acinetobacter baumannii, and various phages.
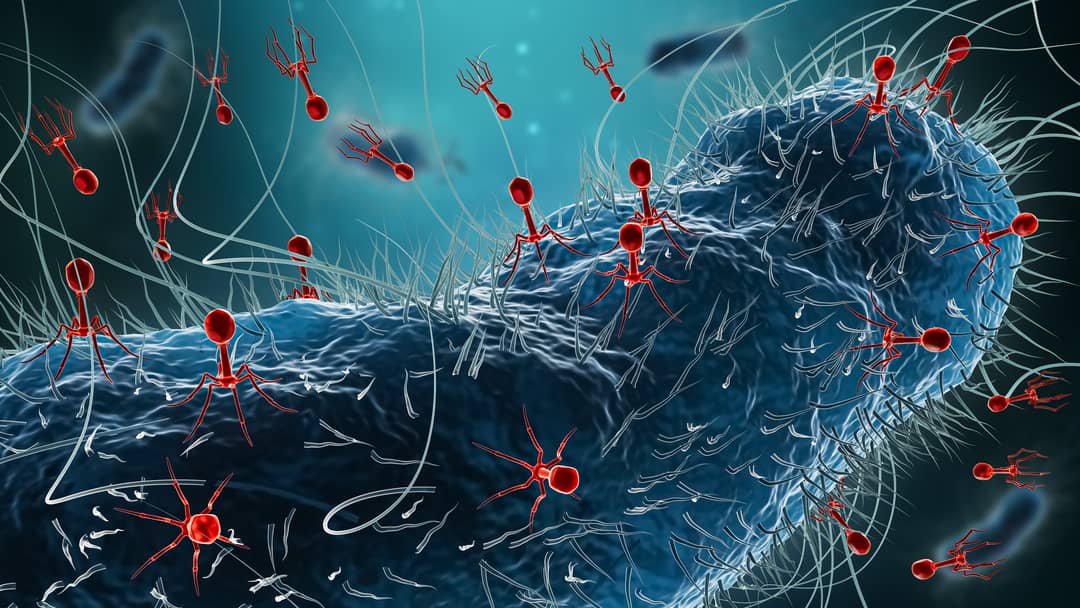
Phages are viruses that live in our body – they live everywhere – and can destroy bacteria. In medical science there’s an influx of emerging research on these curious things that harbour huge potential to beat the dangerous superbugs.
These viruses are Dr Gordillo Altamirano’s specialty. He’s a young doctor, microbiologist and researcher from Ecuador who last year completed his PhD with Monash, of which a landmark new collaborative paper on phages, now published in eBioMedicine, forms a part.
That day in the lab, he was interested in one particular phage and its interactions with A. baumannii. In fact, he became so interested in it he named it after himself – FG02. He’s named other phages after himself, but he thinks this is the one that will be remembered purely because of the way it tricks the superbug.
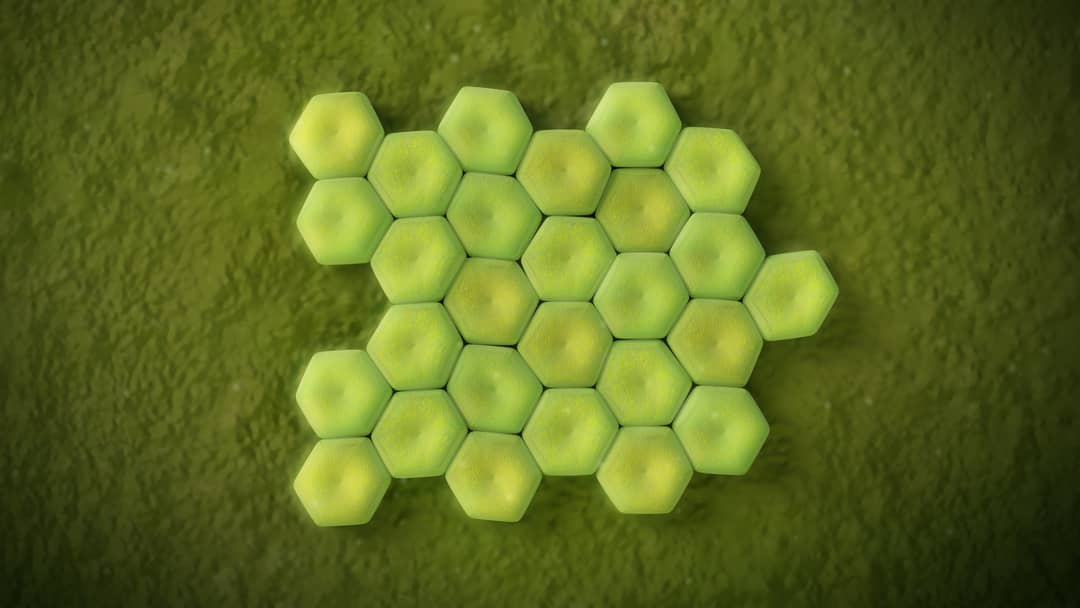
“This superbug – A. baumannii – is interesting because one of the key defences that it has, or one of the things that makes it so resilient and such bad news for patients,” he says, “is that it creates this outer layer made up of sugars called a ‘capsule’.
“The capsule is really useful for the superbug because it’s very sticky, so it allows the superbug to stick to medical devices and to withstand dehydration.
“One of the other uses that the capsule has is that it acts as a barrier. So, parts of our immune system cannot penetrate it and cannot attack A. baumannii.
“The capsule also protects A. baumannii from antibiotics. Because of these sticky, beautiful capsules … it makes this a very sneaky and very smart superbug.”
Read more: Sleepwalking towards an antibiotic apocalypse
According to the Centers for Disease Control and Infection (CDC), it can “cause infections in the blood, urinary tract, and lungs (pneumonia), or in wounds in other parts of the body … it can also ‘colonise’ or live in a patient … especially in respiratory secretions (sputum) or open wounds”.
“I named the phage after myself … I’m not creative at all! I needed to give it a name, so I just went, ‘Alright, what about FG02?’ I have FG01, two, three, four, all the way to six, but FG02 is the only one that we’ve published substantial data on. This phage is just really easy to work with, and it’s led to this really cool discovery.”
Phages are naturally occurring, and the most abundant biological “things” on Earth, found in soil, oceans, inside humans, in sewage and wastewater – everywhere, in all conditions.
Medicine through the phages
The word “phage” is from the Greek phagein, meaning to “devour” or “eat”. They were first discovered in 1917 and the antibacterial properties were identified, but at the time they were considered marginal for human medicine or treatment, and too hard to purify and store. Antibiotics – via penicillin – were invented in 1928 and fell into mainstream use.
Read more: Inside us, bacteriophages fight a never-ending war on bacteria
Dr Gordillo Altamirano says the 1940s and 1950s was the “golden age of antibiotics”, with the discovery of multiple new families every decade. Yet no significant new classes of antibiotic have been discovered for 20 years, and we face a superbug crisis because humanity’s overuse of antibiotics is driving bacteria to become increasingly immune to these life-saving drugs.
This is especially a concern for last-resort antibiotics that are used for very sick patients in intensive care units when all other bacteria-killing methods have failed.
The new paper by Dr Gordillo Altamirano with Monash’s Dr Jeremy Barr has significantly added to the science by finding – not in humans yet, but in mice – that using phages and antibiotics together against the worst superbug showed “significantly improved” results than either of the therapies alone, and also showed how.
The paper graced the cover of the eBioMedicine journal this month. It explains that phages can recognise target bacteria – “their prey”, says Dr Gordillo Altamirano – through an interaction called receptor recognition.
“It's basically a lock and a key,” he says. “The bacteria has a specific lock, and only the phage with its specific key that is tailor-made for that receptor will be able to attach, and then infect.
“It turns out that the receptor that phage FG02 recognises is the capsule of A. baumannii. The phage recognises the capsule, and it says, ‘I like this capsule, I can enter through here’, and it uses it as a door to enter, and destroy and kill A. baumannii.
“The phage injects its DNA inside the bacteria, and then creates many, many copies of itself, and then it bursts it from the inside. This is its cycle of life. Whenever there's prey, there must be a predator, and something to keep the balance.
“The way I normally explain it is to think of it as, ‘The enemy of my enemy is my friend’. Phages are bacteria’s enemy, and because bacteria can infect humans, the phages can be our allies, our friends.”
What this new paper demonstrates is that the combination of phages plus antibiotics is better than either of those two alone, and how.
In previous work, the researchers showed that phages can kill antibiotic-resistant A. baumannii, but phage-resistant mutants emerged. In the same way that antibiotic resistance emerges, so does phage resistance.
“We have been able to confirm that, even in complex living systems, treatment with our characterised phages – particularly phage FG02 – can reliably steer bacteria towards a phage-resistant variant that is resensitised to antibiotics,” Dr Barr says. “Further research in the field is likely to lead to the discovery of innovative uses of combination therapies using phages and antibiotics.”
Dr Gordillo Altamirano is now involved with a human clinical trial of phages against superbugs led by Monash’s Professor Anton Peleg, Director of the Department of Infectious Diseases at the Alfred Hospital and Monash University.

Last year, the Australian government funded Phage Australia, a network of researchers and clinicians throughout the country. The key centre is in Sydney’s Westmead Hospital, but The Alfred Hospital and Monash University’s Centre to Impact AMR have the lead role in Victoria, and the first phase of the trial involves consenting patients with bacterial infections that have stopped responding to antibiotics.
“They will first be screened by an infectious diseases specialist to make sure that indeed there’s no other thing that can be done for that patient – no other antibiotic, no other surgery, no other procedure, nothing,” Dr Gordillo Altamirano says.
“They’re usually patients that have infections that are complicated to begin with, so patients that have, for example, a prosthetic joint infection, which are particularly difficult because the superbug usually attaches to that prosthetic, or you have a patient that has cystic fibrosis, in which the lungs become an ideal environment for the superbug to start growing and replicating. Those patients will be able to apply to be part of the study, and we will administer phage therapy.
“The idea is to recruit at least 50 to 100 patients over five years, and because it’s at stage one, the first questions that we want to answer are relating to safety. So, does phage therapy have any potentially dangerous side-effects in our patients? So that's what we're doing now – which is really exciting.”





