When Monash University announced world-first COVID-19 research in July – at the height of the pandemic – the crucial behind-the-scenes work of a group of PhD students went largely unnoticed.
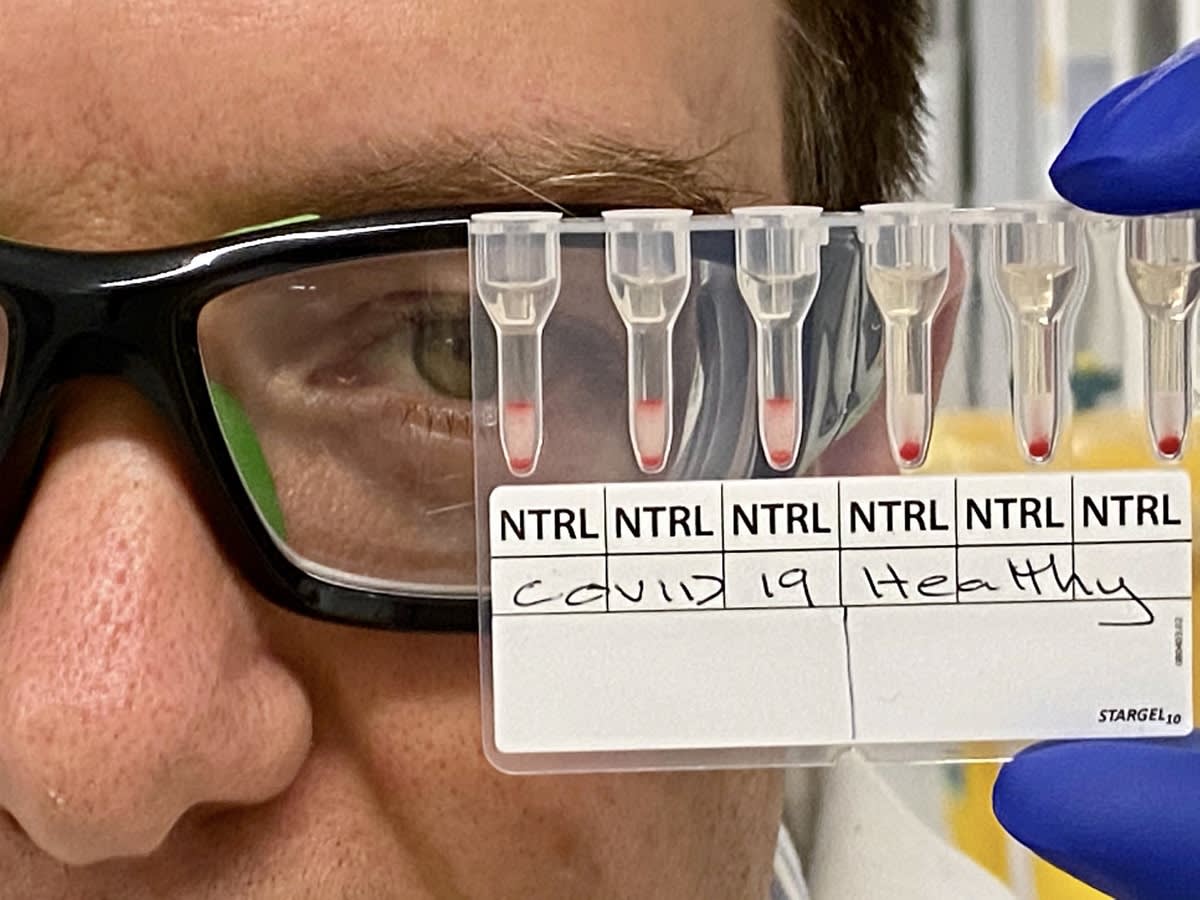
The official announcement was rightly about the scientific breakthrough that has allowed positive COVID-19 tests using blood samples to be carried out in just 20 minutes.
Researchers developed a simple test based on commonly used blood-typing tools; if COVID-19 is in the blood, the red cells agglutinate, or cluster.
Examples of the real-life use of the test would be in contact tracing or in airports or transit points. Using a simple lab set-up, the discovery could see medical teams testing potentially 200 samples an hour. At bigger hospitals with more equipment, that number might be as high as 700 an hour.
It could also help high-risk countries in screening tests, contact tracing and vaccine testing. A patent for the test has been filed.
The research team is continuing work in the lab, but is waiting for funding to commercialise and manufacture the product. The team’s research was published in the journal ACS (American Chemical Society) Sensors.
Professor Banaszak Holl, head of chemical engineering at Monash, commended the work. “We are indebted to the work of our PhD students in bringing this to life.”
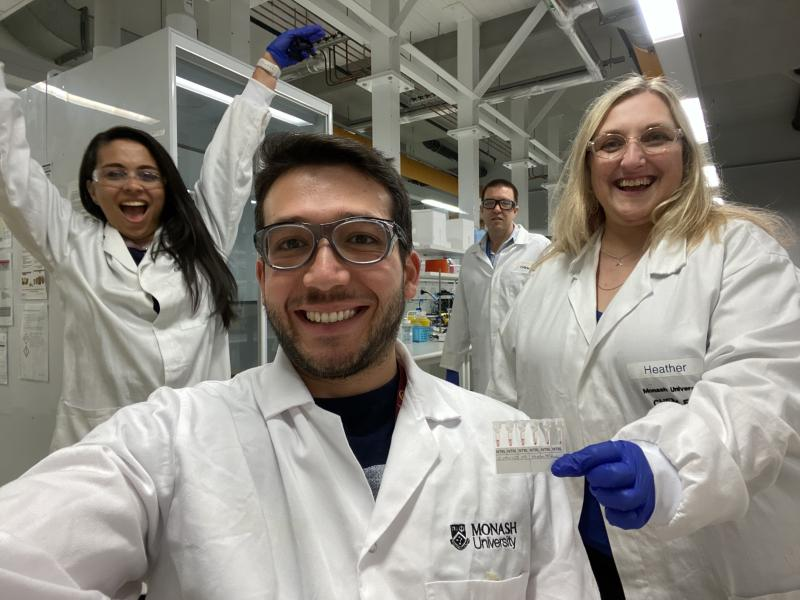
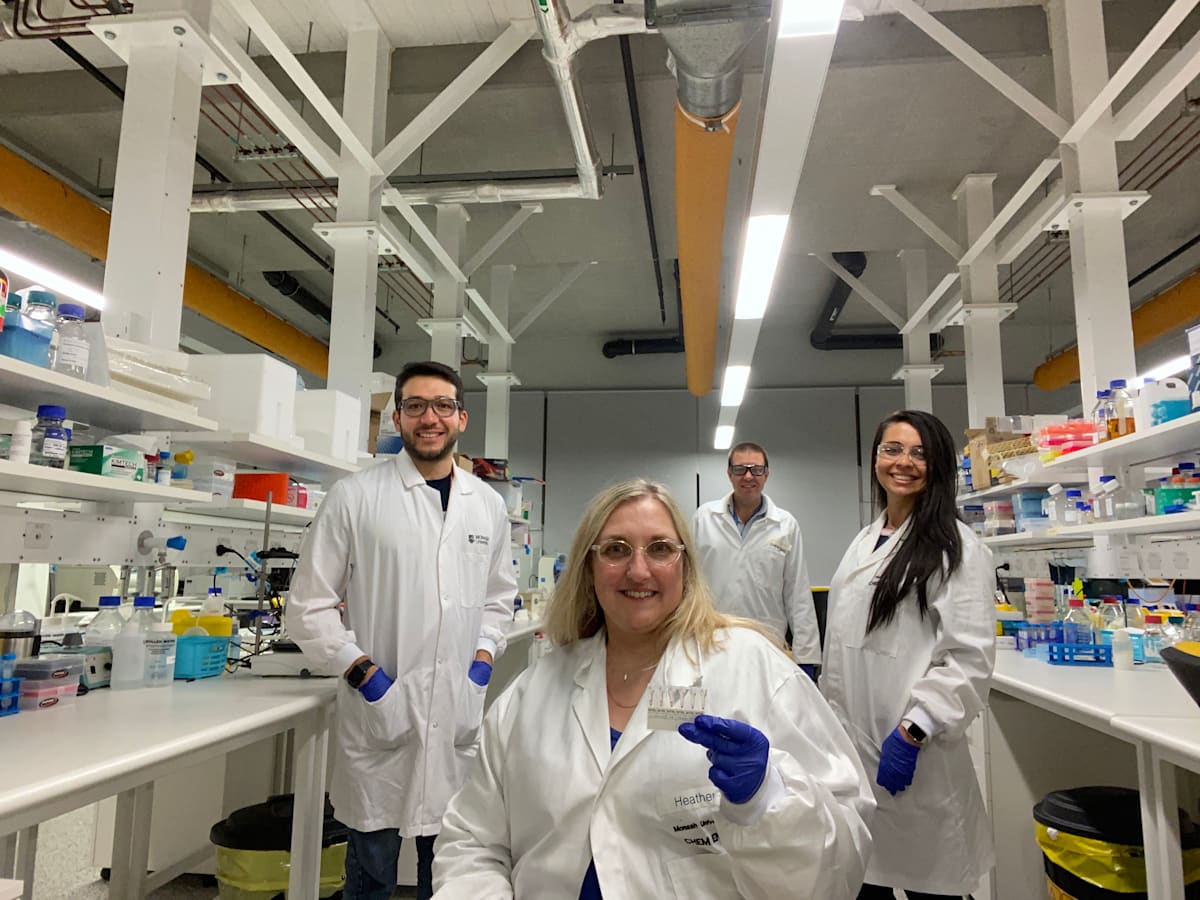
Here are four of those PhD students, all from Chemical Engineering/BioResource Processing Institute of Australia.
Diana Alves
“My supervisor rang me and said, ‘We’re recruiting a taskforce for a COVID-19 project. We’ll do something to help the global community. However, you have to drop your PhD for a few months.’
“I didn’t think twice.
“I knew from this moment on I was being recruited for something very special. COVID-19 had hit my home country, Brazil, very hard. I wanted to not only help Australians, but people from other countries, including my fellow Brazilians.
“My PhD project already worked with blood. I just had to apply what I already knew, such as the preparation of reagents, as well as analysis by flow cytometry and microscopy [measuring how a component sits within a cell].
“The main difference between this and other COVID-19 tests is that this one is cheaper and easier to use. It uses a method very similar to that in laboratories around the world for pre-transfusion testing. People can be tested on a large scale to track cases and isolate individuals with more efficiency and safety.
COVID-19 had hit my home country, Brazil, very hard. I wanted to not only help Australians, but people from other countries, including my fellow Brazilians.
“This COVID-19 test utilises a technology already used in blood banks around the world. Currently, Brazil has more than four million confirmed cases of COVID-19, which has caused 140,000 deaths. There are 2066 services related to blood transfusion, including regional blood banks, in Brazil.
“Hence, by using this cheap and rapid diagnostic, mass testing for COVID-19 can occur throughout Brazil – thus controlling its spread.
“Furthermore, since the test works by detecting COVID-19 antibodies in the blood, we can use it to mass-test participants undergoing clinical trials for a vaccine.
“Not only can this test measure the efficacy of COVID vaccine candidates, but it can also speed up the development of a successful one that could get the world back on track.”
Rodrigo Curvello
“My current PhD is actually very different from this project. I’m developing a low-cost material for the growth of ‘mini-organs’ in the laboratory, generated from biopsies taken from human organs. Currently, an expensive material is required.
“My mission is to develop an alternative that drives the cost down and allows recreation of mini-tumours for cheap and fast drug testing or disease modelling.
“The COVID-19 project was an amazing opportunity to return to my first months of my PhD, remembering all that I’ve learned during my doctoral degree, learn new things from my colleagues and, finally, confirm how multidisciplinary science is.
“I believe this project has enormous potential in this fight against the new coronavirus. The test is robust, reliable, cheap and fast.
“It can be a powerful tool in massive testing of populations. Imagine if Australia could test a large number of people – such as those landing in our airports, or before giving them a vaccine – and get the results in 20 minutes?
“My supervisor, Professor Gil Garnier, called me and said the department was recruiting a few top students to join a multidisciplinary COVID-19 taskforce. The aim was to develop a new serological-based test [a blood test looking for antibodies] to diagnose COVID-19 infections, and somehow contribute to this fight against the deadly disease.
“It can be a powerful tool in massive testing of populations. Imagine if Australia could test a large number of people – such as those landing in our airports, or before giving them a vaccine – and get the results in 20 minutes?"
“I came up with an idea to convert the gel-card-based assay [analysis] into a COVID-19 test. My idea matched with the initial thoughts that Simon Corrie had, so we essentially followed this track.” (Dr Corrie is a senior lecturer in chemical engineering, and a chief investigator in the multi-university CBNS, the Centre of Excellence in Bio-Nano Science and Technology.)
“After that, I got involved in the sample preparations, the proper testing for validation, microscopy, cell labelling, and constant discussions every morning.
“After four weeks of hard work, we had the first positive and negative test in our hands, proving that our hypothesis was true. The whole team was extremely happy, and it resulted in a photo that we named the ‘Eureka Moment’.
Edward Henderson
“The first lockdown had happened, and Dr Corrie gave me a phone call on the Saturday and asked me if I was interested to come in on the Monday for a meeting about a COVID-19 research team. I decided to give it a go ... and from there decided it was something that would be an awesome opportunity.
“My main role was to try and develop a synthetic microparticle assay [analysis] parallel to what the red blood cell assay was trying to achieve, as well as providing input onto the red blood cell assay.
“Our hope was that we would be able to achieve success with the red blood cell test, which was based on previous work in Professor Garnier’s research team, and adapting this technology to a synthetic particle-based system.
“We’re still developing this part of the project, as out of the entire team the large majority were working on the red blood cell test.
“On the first day, at the end of the day, when we had received the project goals, and then spent some time to do some reading and research of the literature, we had a second meeting, and brainstormed ideas and goals. In this meeting, I learned that the people who were part of the taskforce were all experts in their own field, and it showed the power of what a team can do when it comes together.
“The overall experience was amazing, getting to work with such talented people, and the sharing of knowledge and skills was the best part.
“I think this kind of technology has the opportunity to be extremely beneficial in bringing back a semblance of normality in a post-COVID era, where rapidly testing for antibody presence could be useful in a vast array of applications, such as travel, or for analysis of populations.

Vidhishri Kesarwani
“For a person who is passionate about research in the infectious disease space – my PhD was on nanomedicine for bloodstream infections – this seemed like a golden opportunity. How often do you get a chance to be a part of something groundbreaking?
“While Australia and other parts of the world were effectively in lockdown, we geared up in the lab to get this out. The setting of this research was far from a conventional academic environment. It was super-dynamic!
“We had to be swift – understanding the disease context and existing technologies, developing new protocols and performing experiments ... it honestly felt as though we were running a million miles an hour.
“Undoubtedly, the most exhilarating aspect of this research was when the assay [analysis] gave a clear distinction between COVID-positive and healthy human blood samples. Our efforts had come to fruition.
“I’m sure deep down we all knew, at that very moment, that this was going to be huge! It was the hard work, fantastic leadership and sheer resilience that led this team to achieve this monumental result. I am extremely grateful to Simon and our senior academics for giving us this opportunity.
“I truly believe vaccine trials and populous communities with limited contact tracing capabilities and infrastructure would greatly benefit from this research. “
A ‘powerhouse’ team
To Dr Corrie, the team of six Monash PhD students were the “powerhouse” of the intense project who had “bravely agreed to drop their PhD projects at the end of March for an unknown period of time”.
From the experience, he says, they can take the knowledge they can do big, important research work when it matters most.
“They can contribute to a major team challenge, and they can deliver on complex projects in record time.
“This will give them huge confidence going forward in their careers.”





