As medical scientists around the world scramble for answers to the rampant COVID-19 riddle – the pandemic that medicine always feared – a team at Monash University has recycled known tools to find new techniques to test novel coronavirus immunity.
The team, from the University’s Central Clinical School and Alfred Health, has reimagined a set of technological tools to find out who is immune to COVID-19, who remains infectious with the disease, and who is at most risk of developing a severe form. It’s a world-first innovation.
The University’s researchers have started receiving cell samples from Melbourne, as well as the three worst-affected global hotspots – Italy, China and New York. The reason the new test is important, and has been greeted enthusiastically worldwide, is because of the urgent need to determine which frontline health workers are immune, to minimise the number of healthcare workers on temporary leave, and allow workers back into healthcare facilities.

The team’s leader is Associate Professor Menno van Zelm, a young, Dutch-born immunologist who specialises in B-cells, a type of white blood cell central to immune function.
“As we move from needing a test that simply tells whether someone is infected – which is the priority now – to needing a test that can determine who is infectious, who is immune, who is going to get a serious case of the disease, and who will only develop a mild case of upper airway infection,” he said. “This and other tests like it will provide us with a more nuanced approach to managing the disease.”
Health workers to benefit
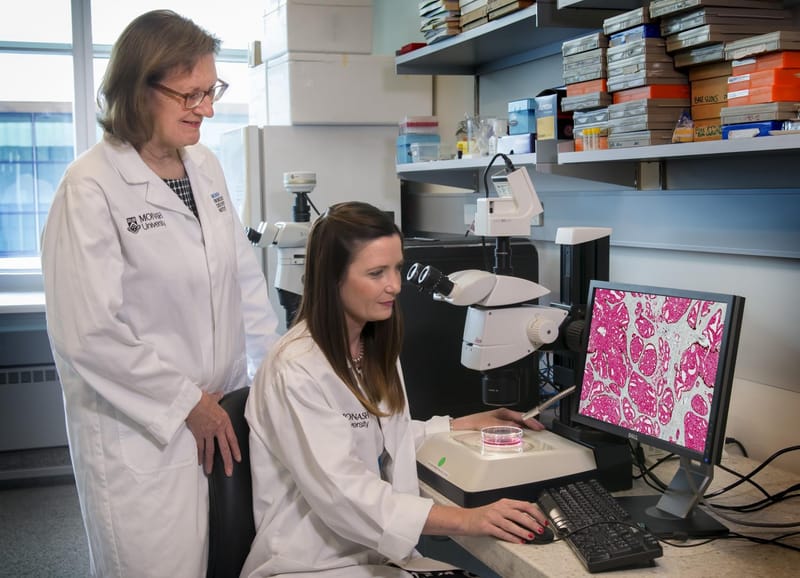
Associate Professor van Zelm’s team worked with Monash University’s eminent Professor Robyn O’Hehir, AO, renowned internationally for her work on allergies and immunity. The project is already being hailed as of potentially huge benefit in testing essential health workers. It should also dramatically help those in vulnerable groups in finding out their exact disease status. The discovery comes as COVID-19 rates soar among medical workers.
“It’s very straightforward to use it in the laboratory. This and other tests like it will provide us with a more nuanced approach to managing the disease.”
The deceptively simple technique seized upon by the researchers is similar to a newly developed test for influenza. It looks at specific B-cells called “memory B lymphocytes”, which are the immune system cells that produce antibodies to fight invaders such as viruses. These cells effectively “remember” pathogens so they can make antibodies more quickly upon reinfection.
The team has made markers for these cells after a COVID-19 infection. Through available technology – a machine called the fluorescence activated cell sorter – they can then count them and use the number to assess immunity.
“It’s very adaptable; we’ve just adopted it for COVID,’’ Dr van Zelm told media after the breakthrough was announced. “It’s very straightforward to use it in the laboratory. This and other tests like it will provide us with a more nuanced approach to managing the disease.”
While there are early signs that the coronavirus curve may be flattening in Australia, governments are concerned that there could still be an autumn-winter surge in cases. The extent of community-based transmission is still unknown. Infections can still occur even after the pandemic curve flattens, because many in the community haven’t developed immunity to the disease.
ICU patients in the trials spotlight
The breakthrough comes as another team of Monash medical researchers play a central role in global human trials of flu and pneumonia drugs on intensive care patients. The team – in Australia, the UK, the Netherlands, Germany, the US, Canada, Saudi Arabia, Singapore, Belgium, Ireland and New Zealand – is testing antivirals, antibiotics and steroids in a bid to outsmart future respiratory pandemics.
There are currently no specific treatments for COVID-19. However, medical scientists are sure some existing drugs for other conditions may have benefits. A Chinese-led study, conducted in Wuhan shortly after the pandemic began to spread, found that the HIV antiviral drug combination lopinavir/ritonavir looked promising in speeding recovery.
It was a small study, but the findings will be fed into a large trial led by a professor of infectious diseases from Oxford University in the UK. That trial will test 30 potential treatments.
Industry joins the COVID fight
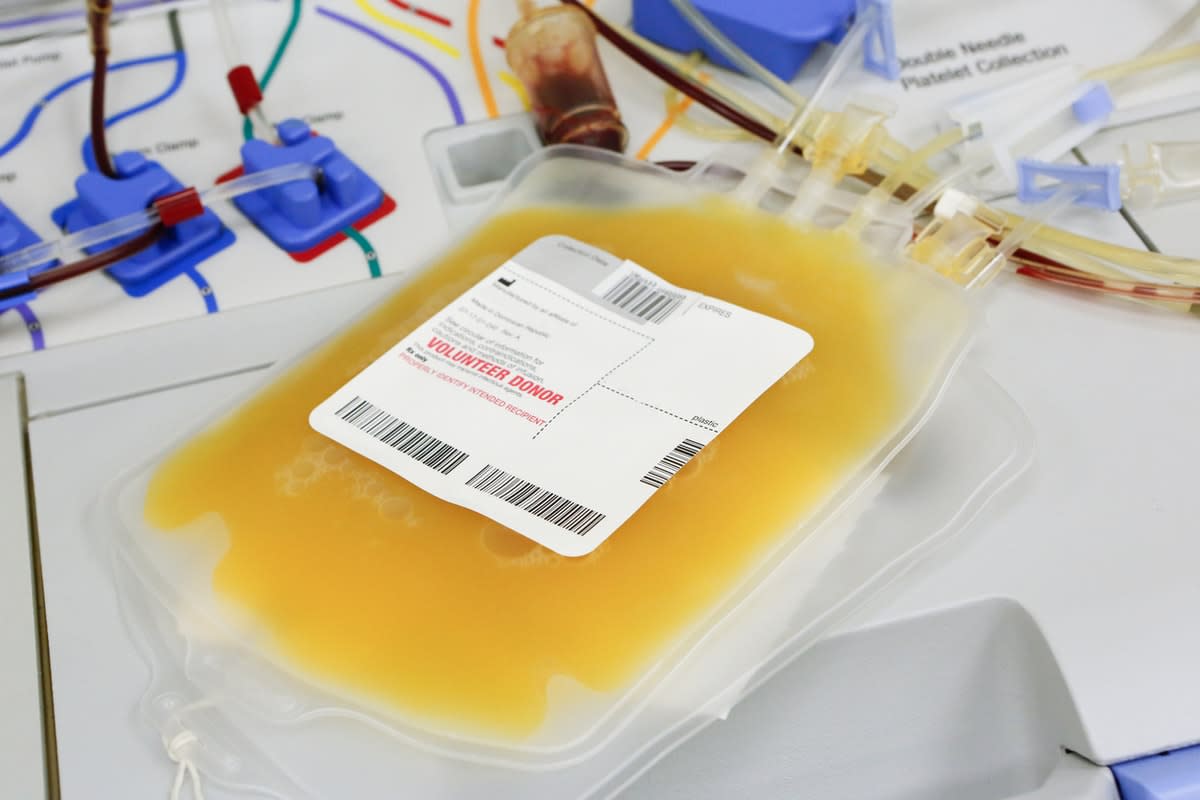
Private industry is also desperately searching for answers. Australian biotechnology giant CSL has announced it will work with its closest rivals in the blood plasma market to develop treatments for patients with COVID-19 complications.
The company said this week it would form an "alliance" with other blood therapy manufacturers in France, Japan, Germany and Switzerland to collect plasma from people who have contracted and then fully recovered from COVID-19, according to The Age.
Meanwhile, the Monash study into B-cells with engrained memory continues. Associate Professor van Zelm said cells from people who had the disease at different severities told complex stories of their own – and may help determine who is immune, who can work, and who cannot.