
When Kate* developed bacterial vaginosis (BV), a vaginal infection that affects one in three women globally, her local doctor prescribed her antibiotics, but the infection kept returning. She then also developed chronic thrush.
Kate was eventually referred to a gynaecologist who treated the thrush and referred her to a BV StepUp trial at the Melbourne Sexual Health Centre (MSHC), part of Alfred Health, which was providing novel treatment to male partners of women with BV.
It was the first time Kate, a final-year medical student, had heard that there was evidence to suggest BV was being sexually transmitted.
The StepUp trial was a multi-centre randomised controlled trial to determine if treating the male partner, at the same time their female partner was being treated for BV, improved the chance of a BV cure.
In the trial, men were given a novel combination treatment of seven days of oral antibiotics, combined with a topical antibiotic cream to be applied to the penis.

The aim of the trial was to determine if this strategy could reduce BV recurrence over 12 weeks, compared to current global medical practice, which is treatment for women only. BV recurrence is extremely high in women with an ongoing sexual partner, with 60-80% getting it back within three months.
Kate attended MSHC and, after seeing a doctor, was diagnosed with BV and referred to the study team, but her partner at the time was reluctant to take part due to healthcare anxiety.
“The clinicians at MSHC and trial staff helped me to navigate this, and created a safe, approachable space. It helped him to understand the purpose of the trial, and how his involvement may relieve the symptoms that I had been experiencing for the past year,” Kate said.
“Within one week of commencing the trial I was symptom-free, and remained that way. The relief was immense not only because the symptoms had gone, but also knowing it was not because I had been doing something wrong.”
With BV now behind her, Kate got on with starting work as a junior doctor.
Several years later, Kate was living and working in a different state and she began a new relationship. Following STI checks, they chose to have sex. Within weeks Kate experienced the return of BV symptoms.
Initially, Kate and her partner went to a GP who prescribed Kate antibiotic treatment. When Kate enquired about the partner treatment, her doctor had not heard of it.
The trial findings had not yet been published, so doctors in the community were still following recommended practice, and prescribing antibiotics to women only. So Kate called MSHC and spoke to the trial team that was running a post-trial implementation study.
Kate was visiting Melbourne, so the team arranged an assessment, and she and her partner were promptly treated.
“I am so grateful for the work and efforts that the StepUp team has done to indisputably show that BV is sexually transmissible and that treatment of all parties in the relationship is required,” she said.
Kate’s case is a typical example of what many women with BV experience, repeatedly. But in contrast to Kate’s story, many do not find a solution or receive a satisfactory explanation about the cause of their recurrent condition. Kate was also fortunate to have supportive and engaged partners who were willing to participate in partner treatment.
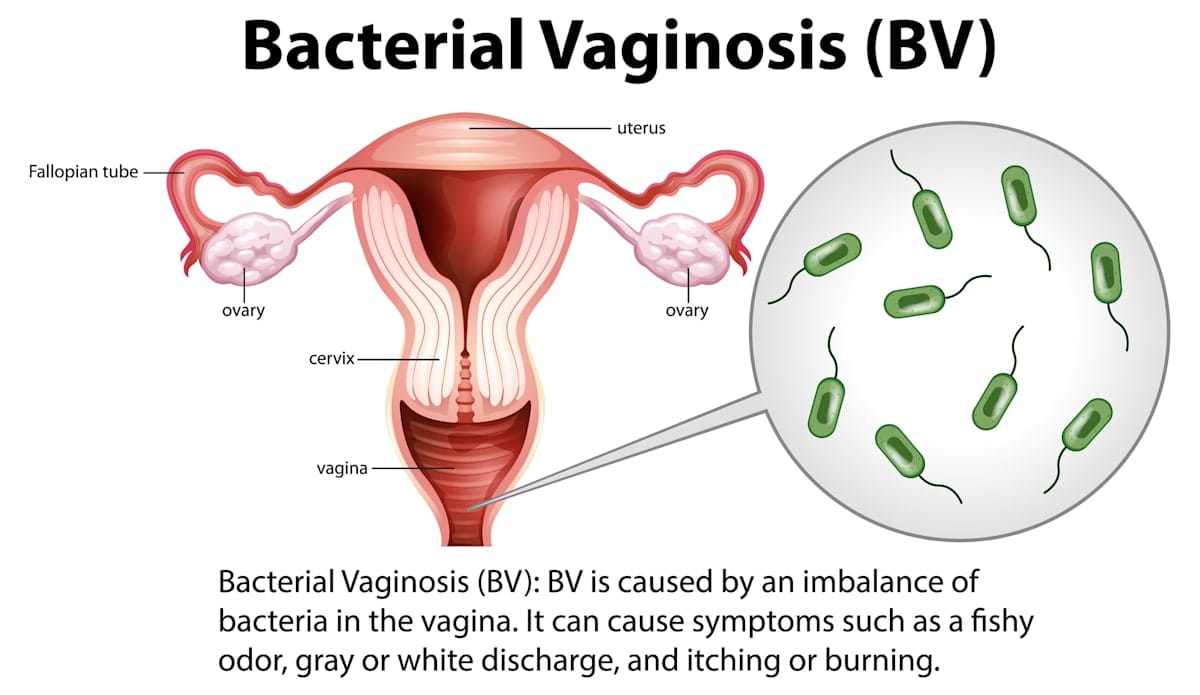
What is bacterial vaginosis?
Bacterial vaginosis is a common vaginal infection affecting one in three women of reproductive age. It’s treated with antibiotics, but more than 50% of women, like Kate, experience recurrence within three to six months of treatment.
Professor Catriona Bradshaw, a clinician researcher at the Melbourne Sexual Health Centre, has been diagnosing and treating women with BV for more than 25 years.
“One of our major challenges in effectively treating BV is that it has been difficult to establish its cause, as no single organism has been exclusively found in women with BV and absent in women without it,” she said.
“BV is really what we call a polymicrobial condition, so a high concentration of different BV-associated bacteria is found in BV. We can visualise the diverse range of bacteria under the microscope, coupled with a drop in healthy lactobacillus bacteria. [The vagina] is actually populated by a small number of lactobacilli that maintain quite a healthy vaginal pH, and a loss of this healthy bacteria means women’s risk of premature birth, miscarriage, risk of HIV, of acquiring all STDs greatly increases.”
She said that for many years now there has been a strong body of evidence to support sexual transmission of BV, and that it “clearly has the profile of a typical STI”.
“BV is not found in women before they commence sexual activity,” she said. “It is very strongly associated with sex, and particularly penile-vaginal sex and lack of condom use.
“Studies consistently show that new cases of BV are associated with new sex partners, and the incubation period is short at just three to four days, just like many bacterial STIs. In contrast, recurrent BV after treatment is far more common in women who have a regular sex partner, suggesting reinfection is a key driver of recurrence.”
Dr Lenka Vodstrcil, an epidemiologist and senior research fellow who co-led the male partner-treatment trial, added that “BV is also very common in women with female partners”.
“We have done studies to show that new-onset BV in women also follows sex with a new female partner, and that the vaginal microbiota of monogamous female couples is concordant.
“Studies by our group and other groups show that women share good and bad vaginal bacteria with each other through their sexual practices. So, we have a strong body of evidence to support sexual transmission of BV between women, as well as men and women.”
The results from the StepUp trial have just been published in the New England Journal of Medicine, and have proven that treating men at the same time as their partner is treated more than doubles the likelihood of BV cure compared to only treating women.

Bacterial vaginosis trial barriers
“BV was initially considered likely to be sexually transmitted more than 30 years ago,” Dr Bradshaw said.
“There were in fact six male partner treatment trials undertaken in the 1980-’90s. They all used varying durations of oral antibiotics in men, but had challenges with their designs and size. Unfortunately, though, they failed to reduce BV recurrence, and this was seemingly the nail in the coffin.
“The failure of these trials was taken by the international community as conclusive evidence that BV is not sexually transmitted. However, reviews of these trials in 2012 and in 2016 concluded that the trials had failed due to limitations, and should not be used as evidence against sexual transmission. But this view failed to get much airplay.”
Dr Vodstrcil said in recent years there had been major advances in molecular tests and sequencing that enabled a better understanding of the range of BV-associated bacteria in women, and also “showed that we can detect the same BV-associated bacteria in men”.
“They are in the urethra – the tube men pee through – and on the penile skin, particularly under the foreskin of men. These BV bacteria are far more common in the male partners of women with BV and are influenced by sexual activity

Dr Bradshaw first became interested in BV during her PhD, and undertook the key trial in 2006 that showed how high BV recurrence was after treatment, and how sex with ongoing partners was seemingly driving BV recurrence.”
“No matter what study we did, we found that the ongoing partner was the key factor always driving recurrence, and no treatment strategy directed at women achieved sustained cure,” she said.
“The lightbulb moment for me was in 2009 when I was reading a trial of male circumcision as an intervention for HIV in Africa.
“A secondary study examining BV showed that the female partners of circumcised men had a greatly reduced risk of developing BV over 12 months, clearly implicating the foreskin in transmission. At this point I began to consider the need for treatment strategies that addressed BV-associated bacteria being present, not just inside the urethra, but also on the skin of the penis.”
Dr Vodstrcil has been working with Dr Bradshaw for 15 years, and over that time has accrued a strong body of evidence that BV, and BV-associated bacteria, are likely to be sexually transmitted, but it did not seem to be widely accepted.
“We were cautious in the interpretation of our data and I ran multiple analyses, and these all confirmed our group’s findings. But we got to a point where we felt we just couldn’t ignore the contribution of males to BV acquisition and recurrence, and we just had to do a male partner treatment trial,” she said.
Dr Bradshaw said it was a breakthrough moment for the team conducting the trial.
“Past trials had not considered penile skin carriage of BV, and now we finally had the evidence from molecular studies and circumcision trials that skin carriage of BV-associated bacteria was likely to be important to target.”
“We felt we needed a strategy that eradicated BV bacteria in men from both the urethra and penile skin. We decided to use a topical antibiotic cream, 2% clindamycin, an approved intravaginal BV treatment for women, combined with oral metronidazole, the oral antibiotic most commonly used in women to treat BV.
“Both drugs have an established safety profile in women, but we needed data to show that these were well-tolerated in men and that the strategy held promise for BV cure.”
The team then conducted pilot studies of male partner treatment among 50 couples that were published in 2018 and 2021.
“The treatments were really well-tolerated in men, and to our delight BV recurrence was unexpectedly low in these couples, and when we tested the vaginal, penile skin and urethral microbiota, we saw a very rapid and sustained reduction in BV bacteria in women and in men,” Dr Vodstrcil said.
The too-hard basket
Dr Bradshaw said researching in this space had been hard because of the perception that BV was “a women’s condition that does not affect the male population”.
“It is also in the ‘too-hard basket’ for researchers and clinicians, as no inroads into cure have been made for decades.
“We would get raised eyebrows and comments from others that we were brave to go down this track, and we entered with our eyes wide open and were prepared to fail.
Bacterial vaginosis affects nearly 33% of women and is often misdiagnosed, despite serious hidden tolls. Dr Jade Bilardi and Dr Catriona Bradshaw of the Melbourne Sexual Health Clinic are putting a stop to it. https://t.co/LwQC1tMhwc#CHANGEIT #MonashLens pic.twitter.com/kbVYEqBY5N— Monash University (@MonashUni) May 23, 2018
Dr Bradshaw said that the team had a great sense of satisfaction that its 20-year journey had achieved something that benefits women and their partners.
“BV is extremely common, and such a distressing, frustrating condition that has been so poorly managed for years. Clinicians and their patients don’t know what to do, and women are commonly subject to endless rounds of antibiotics, which comes at a physical and emotional cost, and is really typified by Kate’s story.
“We have made a major inroad into achieving cure, and this opens up our first genuine opportunity for BV prevention, including developing the first ever tests for men.
“Our next steps involve sequencing the samples from couples to help us determine if there really is a single infectious cause of BV, or whether it’s a polymicrobial infection (caused by more than one organism) from the outset. This work will help us develop better diagnostic tests for women, a diagnostic test for men, and more precise and targeted treatments for men and women.”
The group has developed resources to assist with the implementation of partner treatment. These are available on its website that contains all the information and material consumers and health professionals, including pharmacists, need to understand to be able to prescribe male partner treatment in their clinics and the community.
“We’ve had a lot of interest internationally regarding these findings ,and expect that it will be rapidly adopted by international guidelines,” Dr Bradshaw said.
“If this occurs, then we truly have a genuine opportunity to reduce the burden of BV, and all of its complications, in the community.”
Key partner treatment points
Key points about bacterial vaginosis and male partner treatment:
- Antibiotic treatment is only recommended for women with BV, but up to 80% of women with an ongoing partner experience BV recurrence.
- Male partner treatment involves a seven-day course of an oral antibiotic and a topical antibiotic cream to the penis, both twice daily.
- Treatments are well-tolerated and readily available in Australia.
- This trial confirms that the bacteria causing BV are being sexually transmitted between men and women, and that reinfection of women with BV bacteria is driving the high rates of recurrence.
Professor Bradshaw’s group has received funding from the National Health and Medical Research Council to conduct male partner treatment studies at the Melbourne Sexual Health Centre.
*Source: StepUp website





