With the arrival in Australia of more Pfizer doses, there’s an urgent need to reform the narrative regarding COVID-19 vaccines.
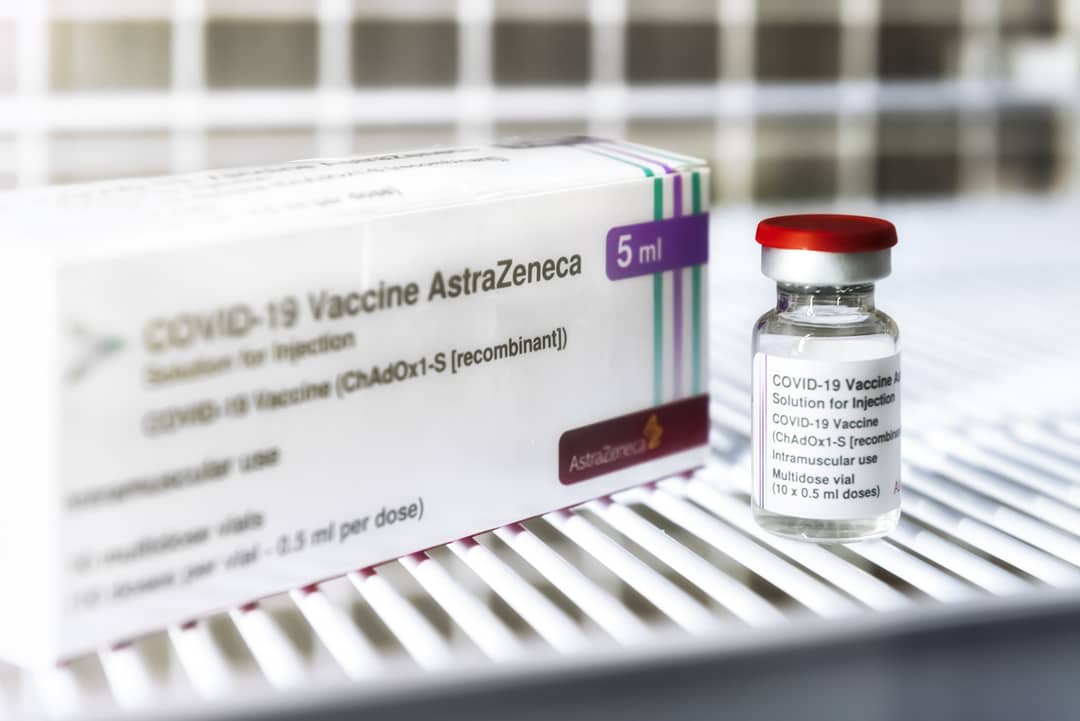
While the locally-manufactured AstraZeneca vaccine is in plentiful supply, it’s the foreign-sourced and still inordinately scarce Pfizer that remains the preferred vaccine for under-60s.
The new momentum behind the vaccination program should not lull us into a false sense of confidence. In Melbourne, for example, the innovative drive-in vaccination hubs are taking appointments for 300,000 AstraZeneca doses and 80,000 second-jab Pfizer doses.
In the meantime, the extended restrictions in Sydney, Melbourne and Canberra have placed about half of the Australian population into lockdown because of our low vaccination rates.
Built into the vaccine rollout in Australia, as well as internationally, is the assumption that wastage of vaccines – between 20% and as much as 50% – must be accepted as inevitable.
This narrative about the inevitability of vaccine losses is the one that must urgently change. The only acceptable vaccine waste should be defined as that arising from considering the safety of patients – namely, when the dose is insufficient, spoiled or expired. All other wastage needs to be eliminated.
The Zero Waste environmental movement has gained traction globally in recent years; as the name suggests, it aspires to dispose of nothing, and the full reuse of resources.
We must learn from this movement in Australia and aspire to the 100% utilisation of COVID-19 vaccines, especially the fragile and expensive Pfizer. Even if we ultimately fall short of this target, eschewing the idea that vaccine wastage is inevitable will surely assist in reducing any squandering of an invaluable resource at a time of enormous scarcity.
In the meantime many states have online appointment booking systems that remain “clunky” and allowed one South Australian to make 40 bookings so he could choose which one suited him best. By failing to cancel the bookings he did not need, he deprived others of getting a jab.
In pursuit of a zero-waste strategy
How, then, can we better go about pursuing a zero-waste strategy in relation to these sought-after vaccines?
It’s clear that the nation’s vaccination hubs are already conscious of the need to avoid waste. There were reports in the media last month of vaccine hubs seeking to administer unused and soon-to-expire doses to anyone willing to have them. These surpluses arise after individuals with scheduled bookings failed to turn up for appointments.
This matter of national importance should not, however, be left to the discretion and scrupulousness of individual vaccination hubs or vaccinators.
There’s an urgent need to introduce universal and comprehensive systems to make sure no dose goes wasted where it could go in the arms of a willing recipient.
One of the most obvious measures that should be implemented rapidly is the institution of waiting lists for all Commonwealth and state-run clinics so that any doses due to be discarded at the end of the day can instead be given to a person who has registered their interest.
One such clinic in Victoria has chosen to run its own list, apparently allowing it to nearly fully utilise its allocated Pfizer doses.

At one point, its waiting list had 198 names. Established waiting lists would be a fair and efficient way of dealing with otherwise expiring doses.
Importantly, it would obviate the need for motivated individuals anxious about COVID-19 to turn up at vaccination clinics at the close of business in the hope of securing a dose that is otherwise to be wasted.
There have been anecdotal reports of this practice in the Australian media as well as abroad, and the author herself is aware of at least one person who has received a dose in this way.
While the ethics of such vaccine-seeking are unimpeachable – it’s preferable that a vaccine is used rather than thrown away – we can surely routinise the process to make sure that near-full utilisation of vaccines doesn’t depend on the motivation of particular individuals and clinics.
Persons vaccinated from such waiting lists should be recorded as such. Creating the category of “waitlisted vaccination” could create wider awareness of any waste minimisation strategy while giving us more accurate records about the extent of vaccine wastage.
The costs of vaccine wastage
Not only is Pfizer imported and scarce, but it’s delicate, and one of the most expensive vaccines against COVID-19.
A zero-waste strategy is worth pursuing because of the enormous tangible and intangible costs associated with our failure to protect the majority of Australians against infection. Every dose that goes into a bin rather than an arm forces the largely unvaccinated Australian population to protect itself with lockdowns.
Wasting Pfizer vaccine is more expensive than wasting AstraZeneca because of the purchasing cost per dose. In November last year, the Australian government bought 10 million doses of Pfizer for US$20 per dose or a total cost of US$200 million ($AUD272 million). AstraZeneca costs about US$4 per dose.
If the reported risk of throwing away 20% of Pfizer at the Melbourne Convention Centre in Melbourne on 18 July, 2021, was to apply to other vaccination centres in Australia, then the cost of binning this first purchase of Pfizer would amount to an economic loss of US$40 million.
A 20% wastage of 10 million doses also means that two million Australians would miss out on their first dose of Pfizer – and two million Australians represents 38% of Sydney’s 5.3 million residents, currently suffering from an extended lockdown and rising case numbers and deaths from COVID-19.
Protective lockdowns are the largest tangible cost of vaccine wastage. Estimates show that the daily cost of lockdowns is between A$100 million and A$125 million a day.
Never has it been more urgent to vaccinate as many Australians as possible, and to ensure that vaccine wastage is as close to zero as possible.
At the lower figure of A$100 million a day, a week of lockdowns costs A$700 million, which is 2.6 times more than the cost of the November 2020 purchase price of 10 million Pfizer doses.
On 19 August, 2021, Melbourne marked its 200th day of lockdown since the pandemic began – the minimal economic waste, assuming the daily cost of $100m, is about $20 billion.
As with environmental waste, it’s the intangible costs that are the hardest to bear. Lockdowns destroy business confidence, and make it especially difficult for small firms to recover sufficiently before the next lockdown.
Then there are the many emotional, psychological and health problems caused by economic insecurity, the loneliness of people living in isolation, and the greater risks of domestic abuse.
The cost of every life lost prematurely to COVID-19 is hard to accept, as is the debilitating impact of long-term illness caused by “long COVID”.
Never has it been more urgent to vaccinate as many Australians as possible, and to ensure that vaccine wastage is as close to zero as possible.
We’re now living through a new wave of the pandemic, with the Delta strain being more transmissible than all previous strains.
The newly-emerging Delta Plus and Lambda strains are much more infectious than Delta, and make the prospects of another pandemic wave especially frightening. At the same time, new Australian government purchases of Moderna, perhaps the most expensive of all COVID 19 vaccines (up to $50 per dose), will entail even larger economic losses if vaccine wastage is tolerated.
The zero-waste objectives of the environmental movement could be emulated in the COVID-19 vaccine rollout to the benefit of all Australians.
This is especially important given that Australia is about to receive 4.5 million soon to expire doses of Pfizer from Singapore and Britain in vaccine swaps organised to coincide with expanding our vaccination program to 16-29 year olds.