The COVID-19 pandemic is a narrative being told by its numbers. By ship. By city. By state. By nation. The world.
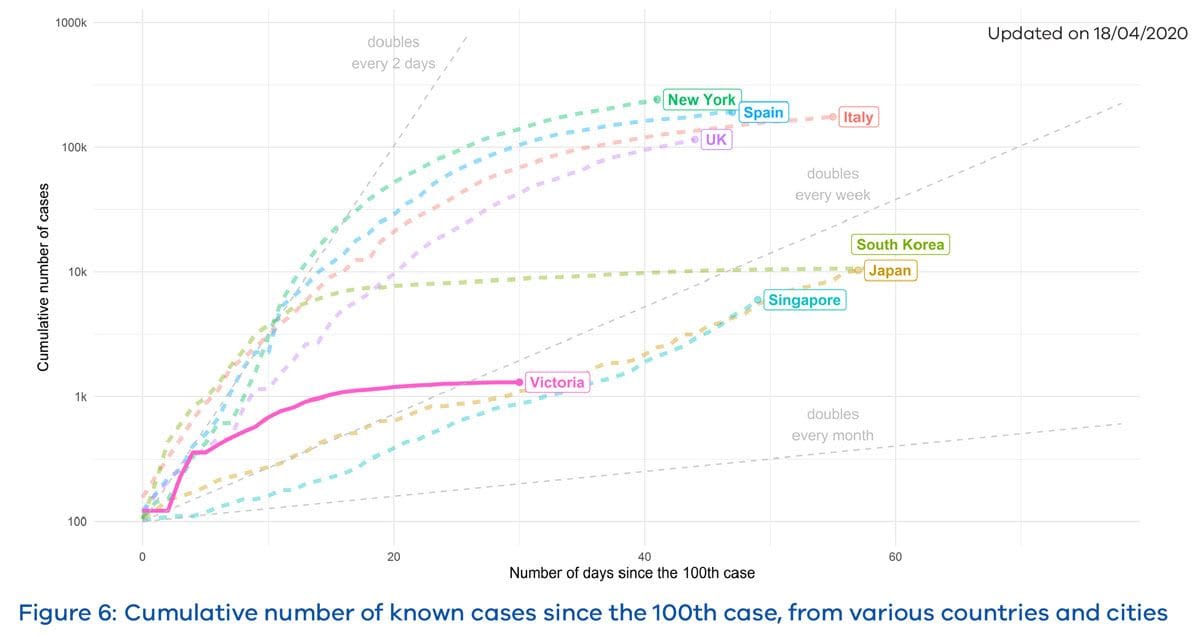
It’s measured by trajectory, and the trajectory of COVID-19 in Victoria has changed dramatically since Stage 3 restrictions were introduced in late March.
On 23 March, when Stage 1 restrictions came into effect in Victoria, we had 460 cases of infection, rising fast, much like the rest of the world. By the time Stage 3 restrictions (among them physical distancing, business closures, and instruction to work from home and stay at home) were introduced a week later, that number had doubled, and the immediate future was uncertain and scary.
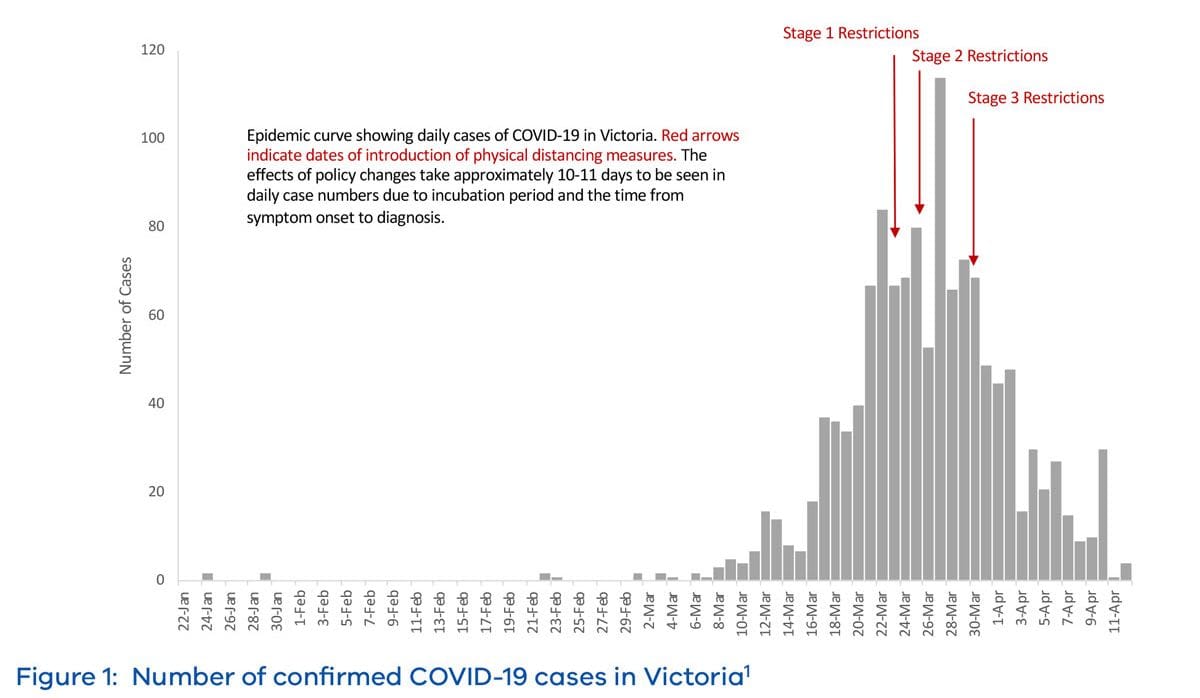
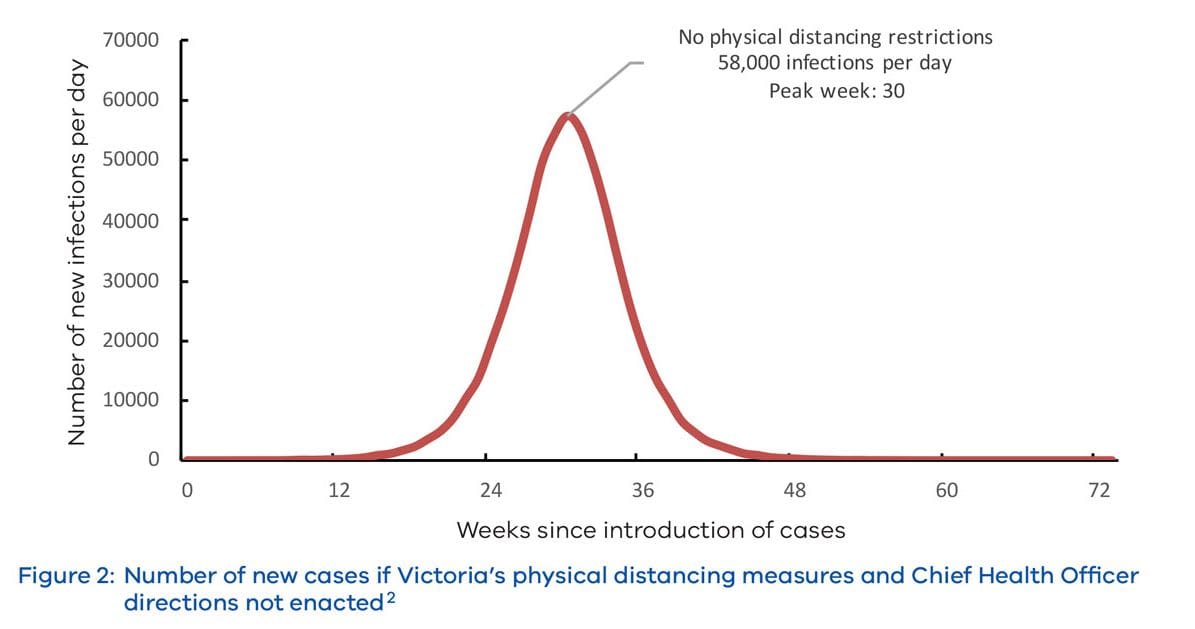
Now we know, broadly, what those numbers could have been without the measures taken.
The Department of Health and Human Services (DHHS) has released modelling to provide greater understanding of the spread of the coronavirus in Victoria.
The modelling was carried out by Victoria’s epidemiological experts at the DHHS, in collaboration with Monash University and the Doherty Institute.
It shows that, without the measures put in place, Victoria’s potential death rate would have averaged 70 a day, and up to 650 deaths a day at its peak. Under this modelling, up to 36,000 Victorians would have died.
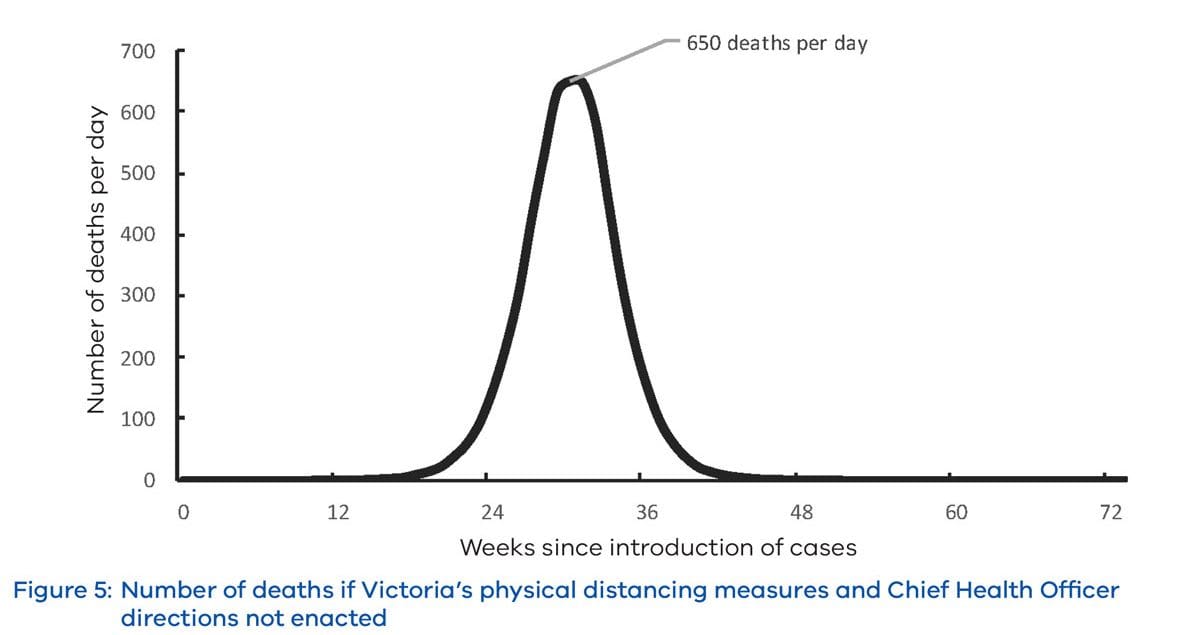
As it stands, Victoria has recorded 15 deaths at the time of writing, with seven new cases over the past 24 hours.
The modelled number of daily coronavirus cases if only quarantine and isolation measures were in place could have hit 58,000 cases per day at the peak of the outbreak.
As remarkable as Victoria’s – and Australia’s – success has been so far, it only requires a glance overseas to heed the warnings that now is not the time to relax too many of the restrictions.
America’s number of infections and deaths continues to rise sharply, and Singapore and South Korea, two countries lauded for their approach, are also experiencing spikes. Indeed, the World Health Organisation has just warned that “ the worst is yet to come”, referencing that the African continent is yet to feel the full COVID-19 fury.
One of the key metrics associated with new case numbers is the effective transmission rate, known as Reff. Using the number of cases observed over time, and knowing how many of them were acquired, along with some information about how long an individual could be infectious for, we can estimate how many people (on average) each infected individual is passing the infection onto.
Read more: COVID-19: Understanding – and misunderstanding – epidemic models
Estimates released by the Peter Doherty Institute for Infection and Immunity have shown that the effective transmission rate is less than one for Victoria. This means that on average, each person is passing on the infection to less than one other person, and so given enough time, the virus could disappear completely.
It’s too early to return to ‘normal’
Countries including Japan and Singapore have started relaxing restrictions, only to see a second wave of the virus hit. Closer to home, in northern Tasmania, we’ve seen how quickly an outbreak can grow if it goes unchecked.
The Department of Health and Human Services mathematical modelling has shown that, if all restrictions were to be lifted, within just three weeks our cases could multiply by more than six times, resulting in a potential 151 people in ICU, and 72 deaths.
Many countries and jurisdictions around the world would love to be in the place that Victoria is in – debating about whether we can play golf, and when our children can go back to school – but instead, they’re having to decide where to set up temporary hospitals, and how to process hundreds of deaths every day.
As Victorian Premier Daniel Andrews said on Monday, relaxing restrictions now will just take options off the table for later.
Where do we go from here?
Our current physical distancing policies have been very “broad brush”, which was necessary at the time when we lacked the understanding of how many people had COVID-19, and where they were located.
Since then, the ability of the state to detect cases and monitor close contacts has increased dramatically, and our health system capacity is continuing to expand. These are key factors that mean restrictions could potentially be gradually unwound.
Now that the spread of COVID-19 appears to be relatively under control in Victoria, at least for now, the narrative has moved quickly to understanding what can be lifted, and what impact it will have on transmission.
The problem is that we don’t have any certainty about what lifting certain parts of restrictions will do to transmission.
While it feels like an eternity, we must remember that COVID-19 has only been known to us for four months. Information is coming rapidly, but we’re still in the early days of our knowledge.
While it feels like an eternity, we must remember that COVID-19 has only been known to us for four months. Information is coming rapidly, but we’re still in the early days of our knowledge.
This is one of the primary purposes of computational biology and mathematical modelling – helping to understand systems when data is scarce, by quantifying uncertainty, and understanding sensitivity to changes in a system.
So far, the physical distancing policies have been integrated into COVID-19 models as a single number that reduces modelled transmission, which we can think of as a sum of all the effects (the broad brush approach).
Now, models are being constructed to better understand this number’s component parts, such as school closures, sporting events, gatherings of more than two people, and many more.
For now, though, returning to normal could be disastrous.
The modelling paints a clear picture: Stay home, protect our health system, and save lives.





