In September 2016, the antimicrobial resistance (AMR) crisis was described by the World Health Organisation’s Director-General, Margaret Chan, as a “slow-moving tsunami” and the United Nations Secretary-General, Ban Ki-Moon, said that it threatened to “make high quality universal health coverage more difficult, if not impossible” and would “undermine sustainable food production”.
It was the fourth time in history that the UN General Assembly addressed a health issue, the other three times being against HIV, Ebola, and non-communicative diseases.
Antimicrobial resistance is a global crisis that threatens to take us back to a pre-penicillin era, where minor infections run the risk of long periods of debilitation or death. Multi-drug resistant diseases, such as tuberculosis, are already epidemics in many parts of the world, and it’s estimated that by 2050, AMR could be responsible for more than 10 million deaths a year worldwide.
Antimicrobial resistance is a phenotype of disease-causing bacteria and fungi that make them able to resist the curative effects of the medicine that we use to treat them. This phenotype emerges and spreads as an evolutionary response to our use of antimicrobials and especially antibiotics, which are most commonly used to treat bacterial infections, and anti-fungal drugs, which are used to treat life-threatening fungal infections.
Professor Trevor Lithgow, from Monash University’s Biomedicine Discovery Institute (BDI), said with society “using more and more drugs, we’re seeing each of these drugs start to fail”.
“We’re losing an evolutionary battle, and we should know better. A growing list of species of bacteria and fungi are displaying resistance to the few drugs that we have left to call on. We are effectively training the microbes to survive the otherwise deadly effects of these drugs.”
The problem is widely attributed to the over-prescription and overconsumption of antibiotics by humans, but the overwhelming majority of the world’s antimicrobial use is in farming of livestock and crops.
“One of the major sources for antimicrobials entering the environment is on farms,” Professor Lithgow says.

“Although attitudes and practices are slowly shifting in Australia, it is still the case globally that livestock industries use antibiotics pre-emptively on chickens, pigs and other animals, and farms also use anti-fungal sprays pre-emptively on crop plants.”
Professor Lithgow nonetheless says that he’s optimistic about how a change in community and industry habits would affect the resistance rate.
“It’s our behaviour that is selecting for antimicrobial resistance phenotypes, and if we change our behaviour, we’ll change the evolutionary pressures, and see antimicrobial sensitivity return to organisms in the environment. This would be true in agricultural environments as well as hospital and healthcare environments.”
“Antimicrobial stewardship” refers to the responsible use of infection-treating medication. It means that antibiotics ought to be used against infections only when needed. It also provides direction for healthcare providers and the community to change their health and lifestyle strategies to decrease chances of infection, and promote healthy immune systems to take care of minor infections as much as they can.
“This is a crucial point,” says Associate Professor Ana Traven, Head of the Laboratory for Fungal Pathogenesis at the Biomedicine Discovery Institute.
“Our latest work is showing us that relatively simple interventions to boost the immune system against fungal infection can have a positive outcome on the chance for recovery.
"There are far fewer anti-fungal drugs available than there are antibiotics, so that research into alternative means to treat systemic fungal infections is a very important recourse to saving lives in the face of evolution of antimicrobial-resistant fungal pathogens."
This research is made all the more challenging because drug resistance doesn’t just give pathogens an advantage against our medicine. It can also give them advantages against our immune systems.
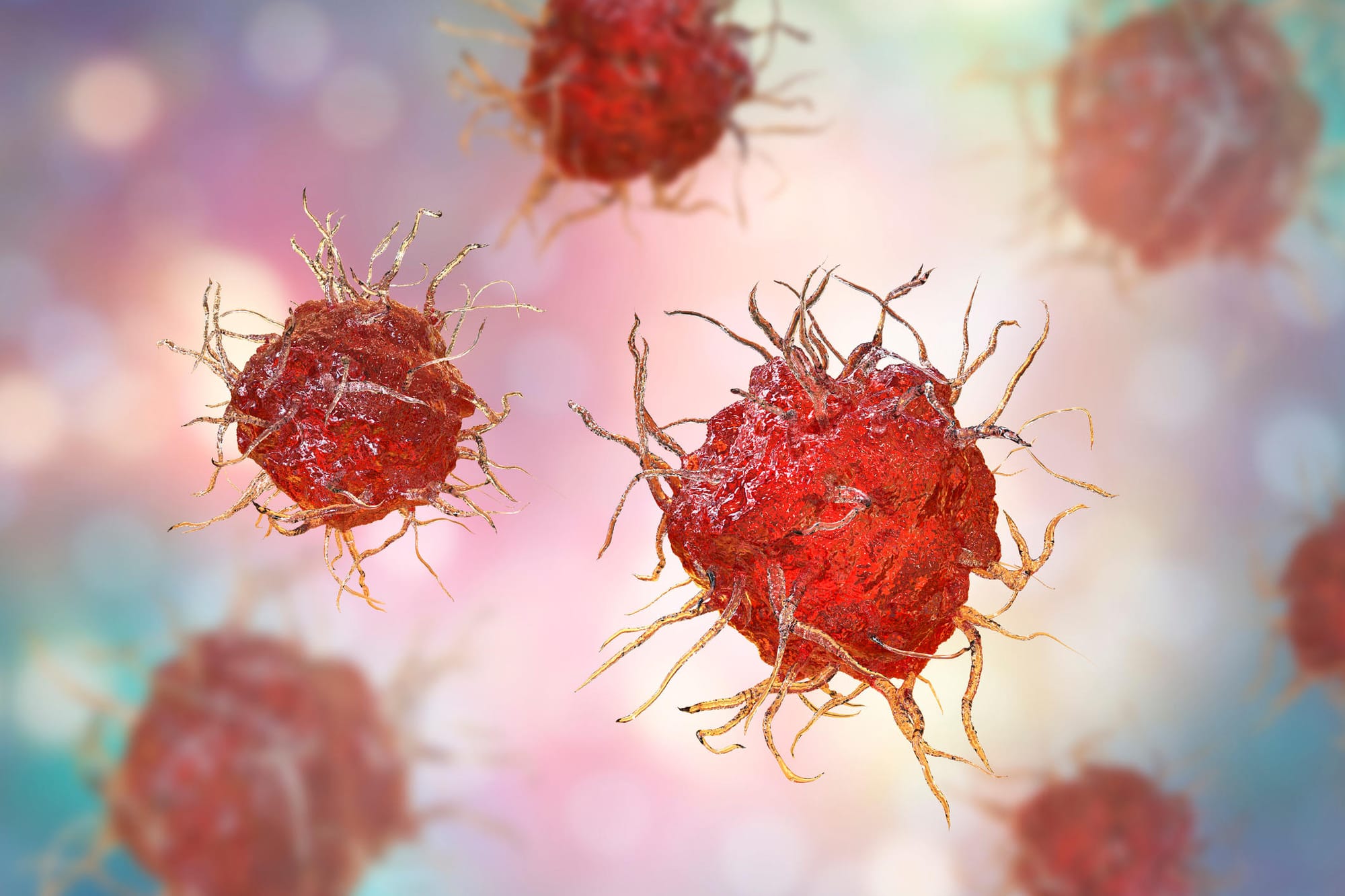
Associate Professor Meredith O’Keeffe, a Senior Research Fellow and Head of the Laboratory of Dendritic Cell Immunity in Health and Disease at the BDI, explains that some drug-resistances can double as ways of avoiding detection by dendritic cells, which play a vital role in recognising infections and mobilising the immune system.
“What we wanted to know was what happens when we take these pathogens before seeing any antibiotics and after when they’ve become resistant; is there a difference in how the dendritic cells see these bugs?
“What amazes me is that it’s black and white. Dendritic cells respond really well to Staphylococcus aureus, and even to MRSA (Methicillin-resistant Staphylococcus aureus). But when antimicrobial pressure selects for resistance to last-line antibiotics, the dendritic cells have a hard time responding to them. And we’re trying to find out why.”
She says this revelation provides a new angle for attack against AMR diseases.
“Rather than relying on antibiotics, how can we tell our immune system that we’re infected and to fight these things? The idea being that we could develop a stimulus that we could give to people to wake up their immune system.
“The bacteria will find it much harder adapting to the innate immune response than it does in adjusting to the next antibiotic that’s thrown at it,” she says,
There are also alternative drug designs being explored to combat antimicrobial resistance.
Associate Professor Max Cryle, a Senior Research Fellow in the Department of Biochemistry and Molecular Biology at Monash, says drugs can be designed that don’t put survival pressure on pathogens, but target other things like their ability to damage a host or to stop the spread from person to person.
“You have less risks of resistance emerging because you’re not putting as much stress on the bacteria to survive,” he says.
“If you can target virulence instead of targeting life and death, the thought is that you’ll reduce resistance because you don’t have as much of a pressure to become resistant.
“The pathways we’re targeting in the bacteria are not backward-sensed. So the bacterium doesn’t know if that process is being inhibited because that process isn’t essential for life. It’s just something that improves its ability to colonise us.”
There are many known mechanisms that bacteria use to resist our immune system.
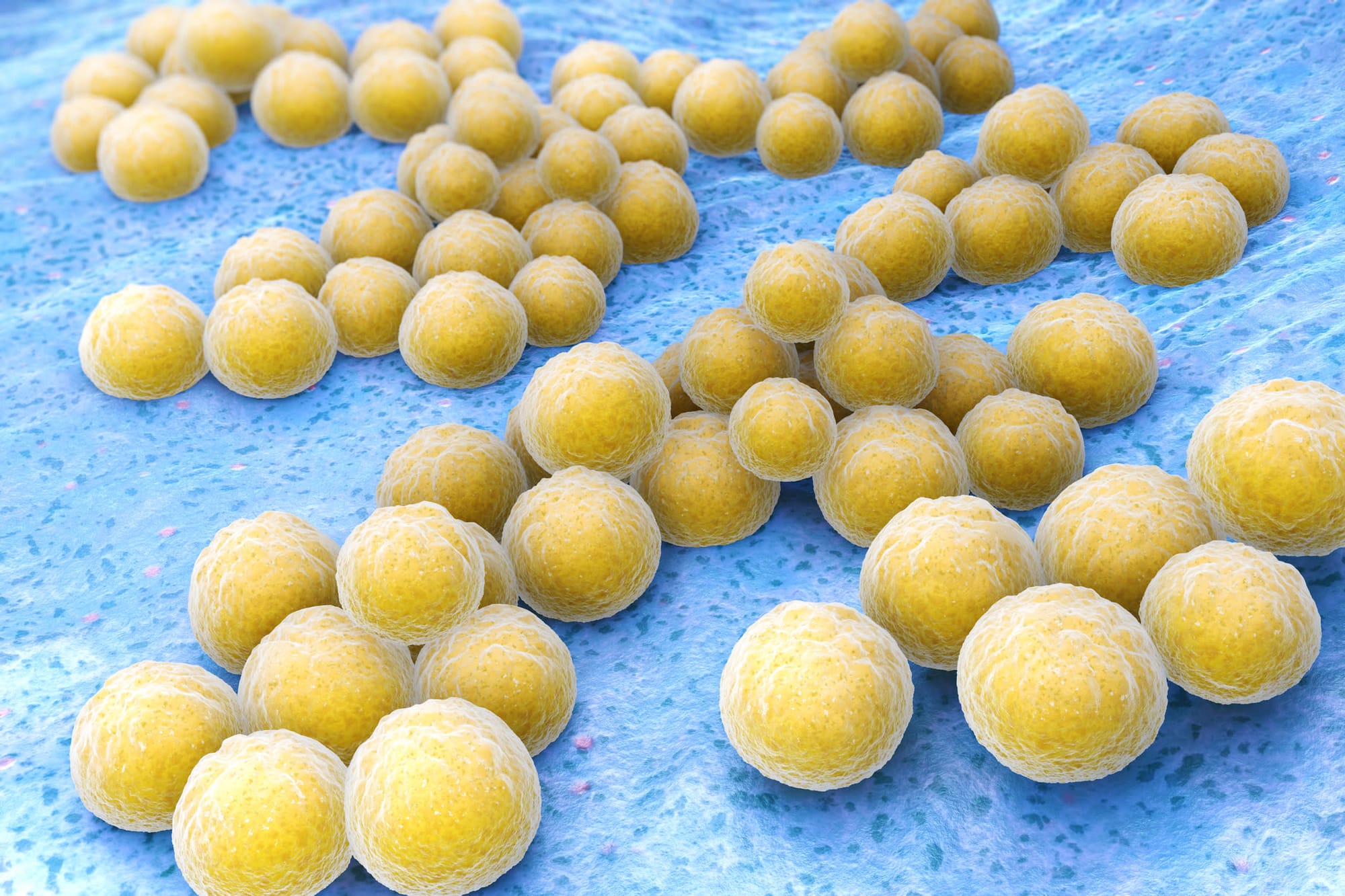
The studies on Staphylococcus aureus, for example, show that this bacteria coats itself in proteins that can protect it from dendritic cells, produces other proteins that disable antibodies, and releases proteases (protein-cutting enzymes) that chop up signalling factors released by our bodies to attract immune “killer” cells.
“If we understand those processes, we can target them in order to weaken the impact the bacteria can have against our immune system,” Associate Professor Cryle says.
“A new antibiotic that we’re working on has a strong affinity for the bacteria’s cell wall, so we can use it to recruit and basically deliver molecules to the surface of the bacterium.
“It’s very hard for the bacteria to change the building blocks that form the cell wall. All of the most worrying strains displaying serious resistance maintain the binding of our antibiotic. In fact, sometimes the resistant bacteria even bind more. There’s very few instances where the binding of our compound is reduced, and these can also be overcome,” he says.
He also outlines the need for drugs that target a specific strain or the smallest number of strains possible so that the drug can be matched with the specific infection.
Traditionally, antibiotics were very broadly targeted and affect not just the disease pathogen, but also the internal microflora of the patient’s body, which could lead to further problems.
“I think with the increasing amount of diagnostics, you can get a much quicker picture of what’s actually causing the problem,” Associate Professor Cryle says.
“I think that will also help create more demand for selective treatment because if you know the causative agent, you can provide treatment that targets that specifically.”
More selectively-targeted drugs would decrease the risk of resistance spreading between different bacteria, he says, because you’d have less communication of genetic material between species of bacteria under the selective pressure.
Bacteria have several mechanisms that let them “share” DNA, so a disease-causing strain of bacteria can acquire resistance from a non-disease species without itself being first exposed to our antibiotics. This is especially a problem in hospitals.
Hospitals have a higher risk of acquiring AMR bacteria. This isn’t just because hospitals are full of sick people. Hospitals need to practice extremely high cleanliness in order to minimise the risk of contamination, but hyper-cleanliness has a disadvantage: greater selective pressure for resistant bacteria.
“Apart from sick people who often have impaired immune systems, there are many selection pressures in the hospital that can drive resistance, including prescribed antimicrobials, and use of disinfectants and antiseptics”, says Professor Anton Peleg, Director of the Department of Infectious Diseases at The Alfred Hospital and Monash University, and Research Group Leader in Department of Microbiology at the Biomedicine Discovery Institute.
“Unwell patients also require more medical device interventions, such as placement of catheters and breathing support equipment, which superbugs like to attach to. These medical devices are life-saving, but do put the patients at greater risk of infections”, he says.
His research team is studying how bacteria attach to medical devices and is developing ways to stop this.
“We all have bacteria on our skin and in our gut, and most of the time we live in harmony. In fact, we need these bacteria for our survival,” he says.
“However, in hospital, people have catheters put through their skin, or a tube put down their throat, or a urinary catheter put in, and these devices all provide a highway for bacteria to invade from their normal place of residence.”
As a consequence of the known increased risks in hospitals, many resources are put into infection prevention. Professor Peleg’s team is developing strategies to help improve practices within hospitals to prevent these infections.

Hand cleanliness, cleaning of equipment and hospital surfaces, sterile procedures, and isolating patients who are at risk of transmitting antimicrobial resistant superbugs are all high priority, he says.
“New strategies are being trialled to prevent hospital-acquired infections such as antimicrobial containing surfaces, hydrogen peroxide vapours, and antiseptic wipes, but old fashioned strategies are also still used such as good old bleach.”
This isn’t a battle that will be won by only immunologists, pharmacologists, or microbiologists, but by the combined knowledge of experts in a range of related fields.
“Traditionally, microbiologists sit over here and immunologists sit over there and never the two shall meet. It’s crazy,” says Associate Professor O’Keeffe.
“You can see that in the BDI initiative which is trying to bring people together in terms of interests from different backgrounds to collaborate in meaningful
ways, rather than ‘I’m in a chemistry department or a biochemistry department.’





