Earlier this year – just after the 2024 football season started – the Australian Football League (AFL) released new concussion protocols for a sport troubled by the injury, and the potentially devastating neurological after-effects.
At the community level of Australian football, the earliest a player can return after concussion is now 21 days. For AFL and AFLW players, it’s a minimum of 12 days before playing again, and only after extensive testing overseen by a medical doctor.
Western Bulldogs player Tom Liberatore has missed six games in 2024 due to concussions. His teammate Ed Richards has already had his second concussion of the new season.
Western Bulldogs midfielder Tom Liberatore will be sidelined "indefinitely" after entering concussion protocols for the second time in three weeks.https://t.co/YgLQyan2gS— AFL (@AFL) May 6, 2024
Footy commentators were also recently questioning the good sense of St Kilda player Rowan Marshall being allowed to battle on after a sickening blow to the head by a West Coast player at the beginning of June.
Protocols for improved detection and management of concussion are rapidly evolving in Australian football, and other sports, but particularly footy, which by nature is more prone to it. However, it’s a complicated area both scientifically and culturally.
The Age reported recently that more AFL players hid symptoms last season, drawing on a 179-player sample from an AFL Players’ Association survey.
A new player survey has produced some worrying data concerning concussion with some players disguising their symptoms. @tommorris32 #9News pic.twitter.com/ZzeLJFovoJ— 9News Melbourne (@9NewsMelb) May 14, 2024
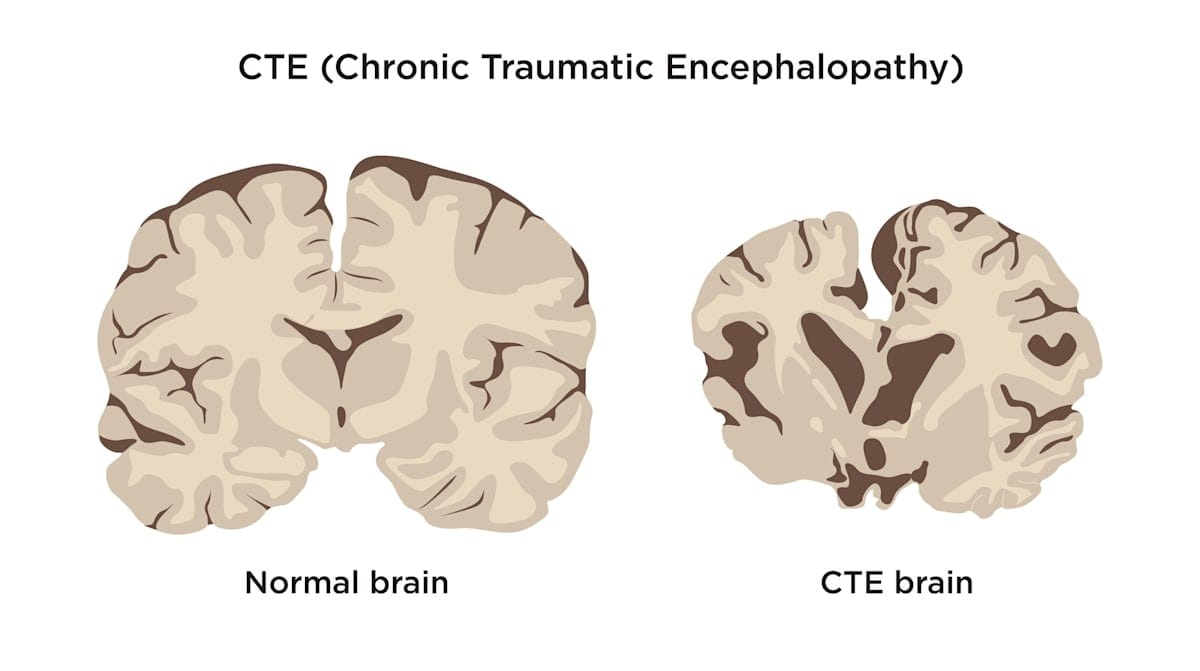
The symptoms of concussion aren’t always short-lived, and a history of concussion is one of the strongest risk factors for sustaining a future concussion. Moreover, links are now becoming clearer between repeated head trauma and chronic traumatic encephalopathy (CTE), a form of dementia.
Now, Monash University researchers have found it’s possible for a blood test to accurately detect the ongoing effects of sport-related concussion in order to help pinpoint when a player can safely return.
The researchers, from the School of Translational Medicine – formerly the Central Clinical School – measured brain-specific proteins in the blood of 81 Victorian amateur footballers who had experienced concussion, and measured them against 56 players who had not.

By repeatedly measuring these proteins in the blood over time, they could then track “neurobiological recovery”, or how long it took the brains to recover.
Until now, there have been no well-established tools for tracking neurobiological recovery after sport-related concussion. The proteins are glial fibrillary acidic protein (GFAP) and neurofilament light (NfL), which are abundant in the brain and released into the blood following brain trauma.

The researchers' paper, published in JAMA Network Open, shows that while most concussed athletes had elevated blood levels of GFAP at 24 hours, about 20% of the cases showed “substantial and persistent” increases in both GFAP and NfL, which remained elevated for more than a month. Those with these extreme biomarker changes were substantially more likely to have lost consciousness as a result of their head knock.
Lens spoke to study leads Dr Stuart McDonald (Monash Trauma Group Principal Investigator) and Dr William O’Brien.
Is this the first time anyone has used a biological tracking tool for neurobiological recovery in sports concussion?
The first time with such a comprehensive approach, yes. We assessed brain-specific blood-based biomarkers which we and others have investigated previously, but the unique thing about this study is not the measure, but how many times and how consistently we did it – eight times over six months for 137 athletes, 81 with concussion and 56 without.
We had very few missing data points due to our dedicated participants and our approach of visiting them for blood collections. The result was a very thorough profile of the trajectories of these biomarkers over time – this had never been done before.
Would the results be translatable to female players, or likely to be even worse for them?
Ongoing work in our lab indicates that these blood biomarkers have utility in men and women, but in this study, we weren’t able to investigate potential sex differences. This is an important area that certainly requires further research, and we hope to provide answers on this soon.
How confident are you that these biomarkers will be able to determine when it’s safe to play again?
We’re optimistic of the potential of these biomarkers for this purpose, but proving it’s safe to play again is very difficult. We know that these biomarkers reflect key components of the brain’s response to injury, and it’s logical that the brain may be more vulnerable to a second injury before these changes have resolved.
Indeed, a previous study from our group using a pre-clinical model found that high levels of NfL at the time of a second concussion were associated with worse outcomes.
So, while we can’t rule out that other factors may be involved in what makes it safe to play again, we have good reason to believe that elevated levels of these biomarkers may indicate a heightened state of vulnerability to another concussion.
How do you see these tests being used?
The most immediate use is likely to aid the diagnostic process. The tests can be used to objectively determine the presence and extent of brain injury, with repeated measures helping track recovery.
While obtaining regulatory approval will take time, our findings provide a more immediate takeaway – concussed athletes that lose consciousness are more likely to have more substantial and prolonged neurobiological changes than those that do not, and may consider a more conservative return to play timeline.
But it’s important to remember that most concussions don’t involve loss of consciousness, and that we found that many concussed players without this feature still had substantial biomarker elevations. Ultimately, we see these tests being used alongside symptom monitoring as a part of the standard diagnostic and return-to-play protocols.
What would this be based on? How do you determine that safe level?
There are two methods. One is via a comparison of biomarker levels to a player’s own pre-injury baseline result – for example, in the pre-season – and the second is using a normative database. In this study we used 56 non-concussed football players, repeatedly tested over time, as a reference point for what is “normal”. We now have a new study underway that aims to create a much larger normative database to help identify what exactly is abnormal.
Do you think the AFL and other leagues will be receptive to the test, given it could result in players having to stay on the sidelines longer than they do now?
We think so. If there’s evidence of some players requiring longer time on the sidelines (as their brain is still recovering), and there’s a TGA-approved method for tracking this, we think professional leagues will be happy to follow the science.
Is there a chance they could actually come back quicker than they do now?
That’s a possibility. For example, a player may have symptoms that resemble a brain injury, but they may be due to a neck injury instead. These tests will only show elevated levels if there’s sufficient trauma to brain cells, resulting in some of their content being released into the bloodstream.
If someone has pure whiplash, it may be possible to use this test to rule out brain injury and instead focus on treating the neck injury. However, developing a rule-out test is complex. We believe the more immediate use of these tests is to rule-in brain injury.
Are these results applicable to other sports?
Certainly. Although the biomechanics of injuries may vary between sports, particularly those with helmets versus those without, the fundamental nature of brain injury remains constant. Regardless of the sport, these biomarkers will show elevated levels following a brain injury, and can be used effectively for diagnosis and monitoring in a similar manner.





