At just 22 weeks, a human baby weighs less than a can of soft drink. A generation ago, these infants were not resuscitated. Today, thanks to major advances in neonatal care, they’re being given a chance at life.
But survival is only part of the story.
“Newborn care has evolved into a true subspecialty,” says Professor Rod Hunt, clinician scientist in Monash University's Department of Paediatrics and director of neonatal medicine and neonatal research at Monash Children’s Hospital.
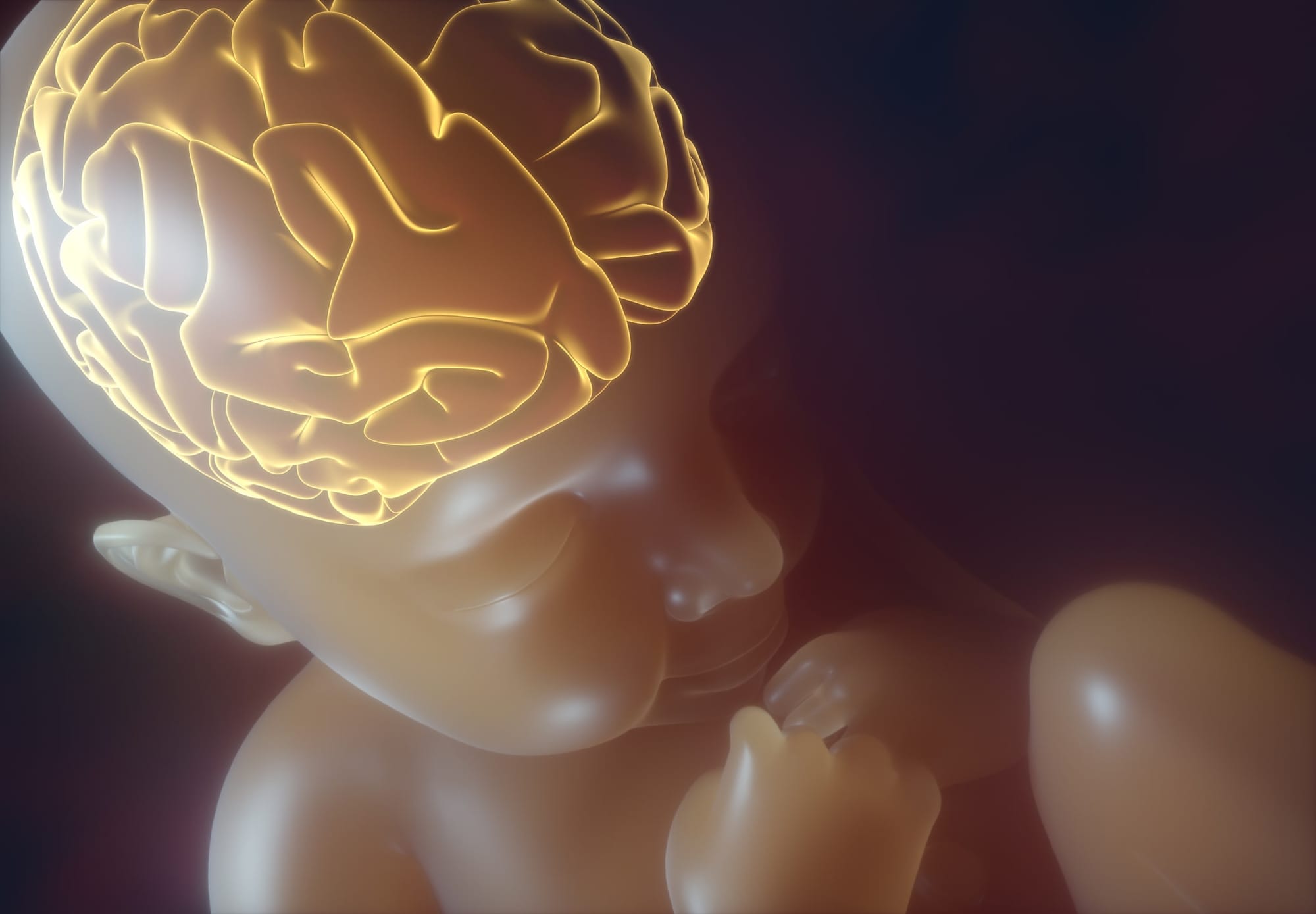
“We’ve made major progress in understanding pre-term physiology and improving our quality of care. But by pushing the limits of viability, we’ve also created new challenges, particularly in protecting the developing brain.”
This complex interplay between survival and long-term outcomes drives Monash’s world-class newborn research program, which has one of the largest neonatal intensive care units (NICUs) in the country, providing both surgical and medical care. It’s considered a cornerstone for neonatal medicine in Australia.
Over the past two decades, and particularly since the establishment of the Financial Markets for Children Foundation’s (FMFC) Chair of Neonatal Paediatrics five years ago, the department has grown from collaborator to leader in multiple national and international trials.
The FMFC is a charitable foundation created by Australia's major financial institutions to fund medical research for children.
From survival to neuroprotection
In neonatal care, the focus has traditionally been on respiratory function.
“The first major advance came from Auckland – steroids for women at risk of pre-term birth, to help babies’ lungs develop,” says Professor Hunt. “The second was artificial surfactant, a soap-like substance that keeps lungs inflated. We learned how to deliver it through a tube, reducing lung injury and saving lives.”
Attention now has shifted to the brain. Monash is leading trials that aim to not only protect pre-term infants from brain injury, but also improve long-term neurodevelopmental outcomes. These include novel anticonvulsants, melatonin-based therapies, and groundbreaking early detection strategies.
Protecting the developing brain
Professor Hunt is currently co-leading the MATILDA platform, an adaptive trials platform in which a number of therapeutic strategies with potential to protect the brain can be trialled in parallel. The first of these will be melatonin as a neuroprotectant in babies with birth asphyxia.
The discovery science underpinning this clinical trial was performed at The Ritchie Centre, a collaborative centre between Monash University and Hudson Institute of Medical Research, making this work truly translational.
Professor Hunt’s team is also pioneering work in the management of newborn seizures. This includes collaborations with Dr Tamara Yawno and Professor Suzie Miller, developing and testing the next-generation anticonvulsants.
“Seizures in newborns can be subclinical,” explains Professor Hunt. “There’s no obvious jerking – nothing visible – but the abnormal electrical storm in the brain is still doing harm. Our tools for detecting and treating these seizures are rudimentary. We’re working to change that.”
These efforts sit alongside other critical work to protect brain development in premature infants.
One area where there’s been significant improvements is cerebral palsy (CP), a condition that originates in pre-term infants in nearly half of all cases. Thanks to improved neuroprotection – including magnesium sulfate for women at risk of pre-term birth, steroids to promote lung development, and early diagnostic tools – rates of CP globally have nearly halved over the past two decades.
“Twenty years ago, CP was diagnosed around age two. Now, with general movements assessments and early detection clinics like the one led by Associate Professor Atul Malhotra, we’re identifying high risk of CP at three to four months,” says Professor Hunt. “That gives us the chance to intervene when the brain is most plastic.”
Associate Professor Atul Malhotra’s clinic is one of the first of its kind in Australia, offering families early assessment and support through a structured, multidisciplinary model.

Preserving oxygen flow, protecting the brain
While much attention is placed on treatments after birth, work by Associate Professor Calum Roberts and Professor Arvind Sehgal focuses on preserving oxygenation and circulation from the very start.
Alongside Professor Hunt, Associate Professor Roberts, head of the Lung and Resuscitation Group and consultant neonatologist at Monash Children’s Hospital, is helping lead the INPRES collaborative, a research partnership spanning Oxford, Parkville and Monash. Together, they design and run clinical trials that improve neonatal intensive care.
One such study is the neoGASTRIC trial, which aims to optimise the way nasogastric tube feeds are managed in the NICU. The intervention tests whether avoiding a common NICU practice – routine aspiration of gastric contents from nasogastric tubes – could lead to better outcomes for pre-term babies. It’s a deceptively simple intervention with potentially global impact.
“The neoGASTRIC trial will include more than 7000 infants,” Associate Professor Roberts says. “It’s the largest randomised trial ever conducted in pre-term infants and it’s on track to complete in just two-and-a-half years. That’s the power of world-leading collaborations like INPRES to rapidly change clinical care.”
Read more: Unlocking the mystery of brain function and connectivity
Meanwhile, Professor Sehgal, who is neonatologist and head of cardiovascular research at Monash Children’s Hospital, is investigating the impact of pre-birth growth restriction on the developing heart and brain.
Birthweight below the 10th percentile for gestational age and sex affects thousands of infants delivered worldwide annually, and recent research is looking at therapies such as melatonin that might be beneficial to the developing heart, brain and lungs.
Since 2007, Professor Sehgal has studied the patent ductus arteriosus (PDA), a small blood vessel essential in fetal life that should close shortly after birth. In pre-term infants, this closure often fails to occur, which can affect blood flow to the brain.
“Managing the PDA successfully is neuroprotective,” he says. “Our work is helping define how and when to intervene, so we can better-support the circulation and brain perfusion in our smallest patients.”
Regenerative therapies on the horizon
One of Monash’s most exciting innovations is the neonatal cell therapy program led by Associate Professor Malhotra, a consultant neonatologist at Monash Newborn and clinician scientist in the Department of Paediatrics and Hudson Institute of Medical Research.
Professor Malhotra leads the only group in Australia currently conducting stem cell and cell therapy trials in newborn infants.
One recent world-first study, CORD-SaFe, showed that using a baby’s own cord blood cells as a treatment is both safe and feasible in extremely pre-term infants. The therapy involves collecting a baby’s own cord blood cells at birth and reinfusing them shortly after – an approach known as autologous cell therapy.
The recent establishment on-site of the Hudson’s Cell Therapies platform has enabled the processing of human cellular therapy products outside the Melbourne CBD for the first time, supporting clinical trials such as these within the Monash Medical Precinct.
In newly-published follow-up data, none of the treated infants were assessed as high risk for cerebral palsy, compared with a 7% rate in the control group.
“We’re not just asking if it’s possible,” says Associate Professor Malhotra. “We’re starting to see signs that it might be making a difference.”
A larger international trial, CORD-CELL, is now underway to test the therapy’s effectiveness in improving long-term outcomes.
Looking to the future
With more than 40 clinical trials in motion, Monash’s newborn research hub is thriving. Investigators are exploring new anticonvulsants, advanced imaging, predictive biomarkers and early interventions across a range of risk areas.
Strong funding support and a deeply embedded culture of innovation underpins this work, fuelled by collaboration between clinicians, scientists and research nurses across the Monash Health Translation Precinct.
Education is a core part of this vision. The newborn team contributes to undergraduate and graduate medical teaching, and hosts placements for students from around the world, helping to train the next generation of neonatal leaders.
“We’re going from strength to strength,” says Professor Hunt. “The brain is the final frontier in neonatal care – and we’re just getting started.”
This article is part of the “60 Years of Impact” series celebrating the Department of Paediatrics at Monash University.





