
Monkeypox, now officially referred to as mpox, is an infectious disease caused by the monkeypox virus (MPXV), which belongs to the orthopoxvirus genus. This genus also includes the variola virus, the causative agent of smallpox.
The first documented case of mpox in humans was reported in 1970 in the Democratic Republic of the Congo (DRC). Since then, mpox has been classified into two primary clades:
- The Central African strain, which is more virulent
- The West African strain, which is generally less severe.
Historically, cases of mpox were rare outside of Africa; however, a significant global surge in cases began in May 2022, and now Sweden has confirmed its first case.
Failure to deal with mpox outbreak ‘is risk not just to Africa but whole world’ https://t.co/Y87B0rfD9W— The Guardian (@guardian) August 17, 2024
This alarming increase prompted the World Health Organisation (WHO) to declare the outbreak a Public Health Emergency of International Concern (PHEIC), highlighting the rapid spread of the virus and its potential for severe health impacts.
Transmission dynamics
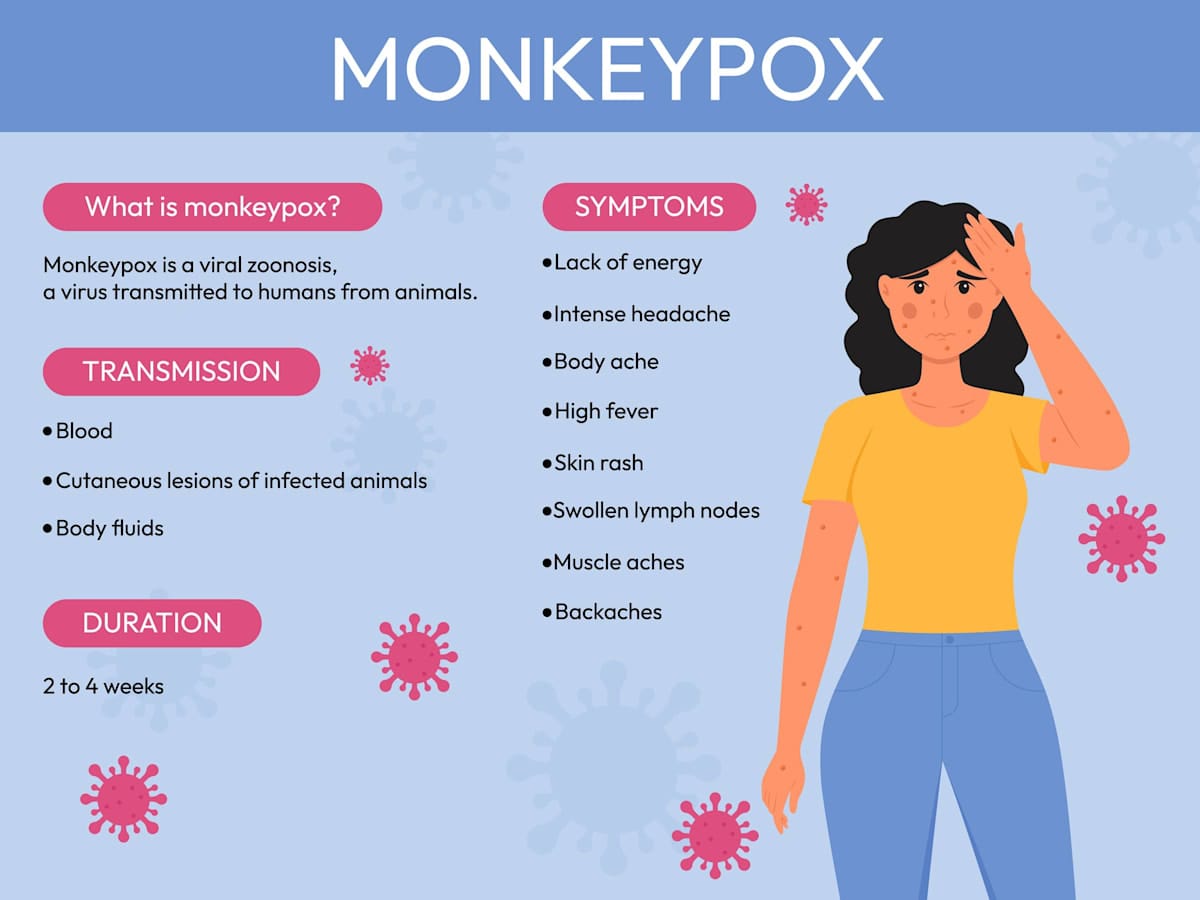
The transmission of the monkeypox virus occurs through several primary routes, with human-to-human transmission being the most significant. This transmission typically involves direct contact with the lesions or bodily fluids of an infected individual, particularly during intimate interactions.
Respiratory droplets can also facilitate transmission during prolonged face-to-face contact. Additionally, fomites – contaminated surfaces – can serve as vectors for the virus.
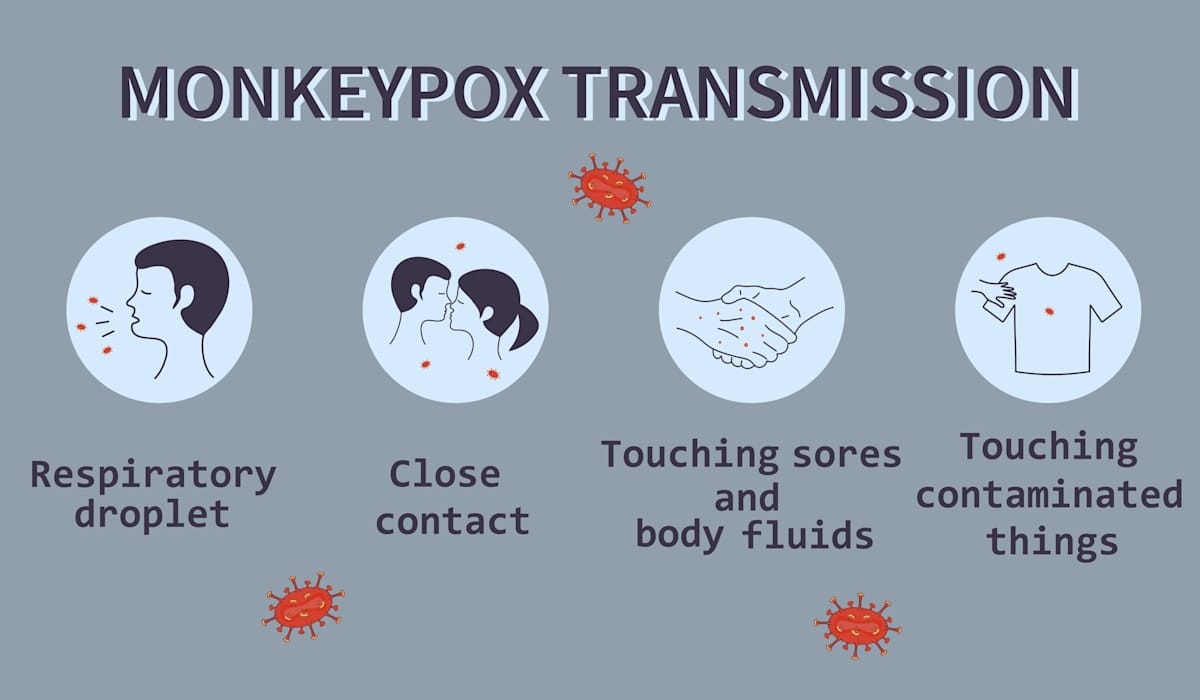
Animal-to-human transmission remains a critical route, often occurring through direct contact with infected animals, such as rodents or non-human primates, particularly in regions where bushmeat is consumed.
Vertical transmission from mother to foetus during pregnancy has also been documented.
The epidemiology of mpox has notably shifted since the outbreak in May 2022, with a marked increase in cases reported among men who have sex with men, indicating a change in transmission dynamics.
The clinical presentation of mpox includes symptoms such as fever, lymphadenopathy, and characteristic skin lesions.
Although mpox is less lethal than smallpox, it still poses significant health risks, particularly to vulnerable populations.
Recent outbreaks and global response
The emergence of mpox cases in non-endemic regions has raised concerns about public health preparedness.
Countries such as Australia are enhancing surveillance and public health education to monitor potential cases and prevent outbreaks.
Mpox infections in Australia have spiked, but we shouldn’t panic. Here’s why. https://t.co/Tq8IoenvVu— The New Daily (@TheNewDailyAu) August 16, 2024
The WHO’s designation of mpox as a PHEIC underscores the urgency of addressing the disease’s potential for rapid spread, particularly in populations with low immunity due to the cessation of smallpox vaccination programs.
In Australia, where widespread immunity against orthopoxviruses is lacking, vigilance is essential to mitigate the risk of mpox entering the country, especially through international travel.
Recent reports indicate that the global mpox outbreak has continued to evolve, with cases being reported in various countries, including those in Europe and the Americas.
The recent emergence of the more virulent Clade I strain of mpox raises significant concerns about its potential to escalate into a global pandemic, particularly in the Indo-Pacific region.
This strain, which has been linked to higher mortality rates and increased transmissibility, has already led to outbreaks in countries including Sweden and Indonesia, with the World Health Organisation declaring it a public health emergency of international concern.
In 2024 alone, more than 15,600 cases and at least 500 deaths have been reported, predominantly from the Democratic Republic of Congo, highlighting the strain’s severity.
The Indo-Pacific region, with its interconnectedness and varying healthcare capacities, could face substantial risks if the virus spreads unchecked.
The presence of Clade I outside Africa, as seen in Sweden, indicates that the virus can cross borders easily, posing a threat to countries with less-robust public health infrastructures.
Current treatment options?
Vaccination strategies for mpox significantly differ between its two primary clades, Clade I and Clade II, due to variations in virulence, transmission dynamics, and outbreak contexts.
Clade I, endemic to central Africa, has a historically higher mortality rate of up to 10% and is primarily transmitted zoonotically, with limited human-to-human spread.
In contrast, Clade II, particularly the subtypes Clade IIa and IIb, has a lower mortality rate of about 3.6%, and has been responsible for the global outbreak that began in 2022, spreading predominantly through human contact, especially within sexual networks.

Vaccination efforts for Clade I target high-risk populations in endemic regions, emphasising rapid vaccination following exposure due to its virulence.
Vaccines such as JYNNEOS and ACAM2000 are expected to provide cross-protection against Clade I, although specific efficacy data is limited.
Public health education on zoonotic transmission is also crucial to prevent outbreaks. For Clade II, vaccination strategies have been more aggressive, especially for Clade IIb, with vaccines such as JYNNEOS deployed in non-endemic regions targeting men who have sex with men (MSM), and other high-risk groups.
This includes both pre-exposure and post-exposure prophylaxis, supported by global efforts to establish vaccine stockpiles and ensure equitable distribution, particularly in Africa, where shortages have been reported.
While both JYNNEOS and ACAM2000 demonstrate efficacy against Clade II, with JYNNEOS showing 100% protection in non-human primate studies, data on their effectiveness against Clade I remains limited.
Additionally, antiviral treatments such as Tecovirimat have been found to be ineffective, highlighting the need for urgent further research into effective therapeutics for mpox management.
Where do we go on from here?
The current global mpox outbreak has underscored critical lessons learned from the COVID-19 pandemic, particularly in the areas of communication, equity, and preparedness.
Effective responses require clear, empathetic communication to build trust and reduce stigma around the disease, especially among marginalised communities disproportionately affected by outbreaks.
Rapid containment measures, including case identification, contact tracing, and isolation, have proven essential in managing spread, mirroring successful strategies from COVID-19.
The pandemic highlighted the importance of leveraging technology for information dissemination, ensuring equitable access to resources.
A coordinated government response is vital, emphasising collaboration across all levels of public health agencies to address emerging inequalities.
Further, the necessity of stockpiling vaccines and ensuring their equitable distribution has become evident, as seen in the challenges faced during the mpox outbreak. Vaccination campaigns must be comprehensive and community-engaged to enhance uptake and address hesitancy.





