
What do you think of when you hear the term “eating disorder”? If it’s a girl or young woman with anorexia nervosa, you’re not alone.
That’s the eating disorder stereotype, but far from the reality. The truth is that people of any age, gender identity, body size, sexuality, or cultural background can be impacted.
Puberty is a normal process that the vast majority of us will go through. It’s also a well-known critical risk period for the development of eating disorders likely due to a range of biological, psychological, social, and environmental changes.
However, there’s another normal transition stage in life for women or people with ovaries, namely menopause, which is, thankfully, receiving more mainstream attention in recent times.
Menopause can increase the risk of the onset, redevelopment, or worsening of an eating disorder. Estimates suggest about 3.5% of people in the menopausal phase are also experiencing an eating disorder.*
The collision of menopause and eating disorders
In midlife, most women will experience some changes in their menstrual cycle with the slowing of ovarian functioning. This phase is called perimenopause, which means “around menopause”, and can occur up to 10 years before menopause.
Menopause is reached at an average age of 51, with some people being quite a bit earlier or later in life, and marks the end of ovarian and reproductive functioning. Post-menopause is considered to be 12 months after the final menstrual period.
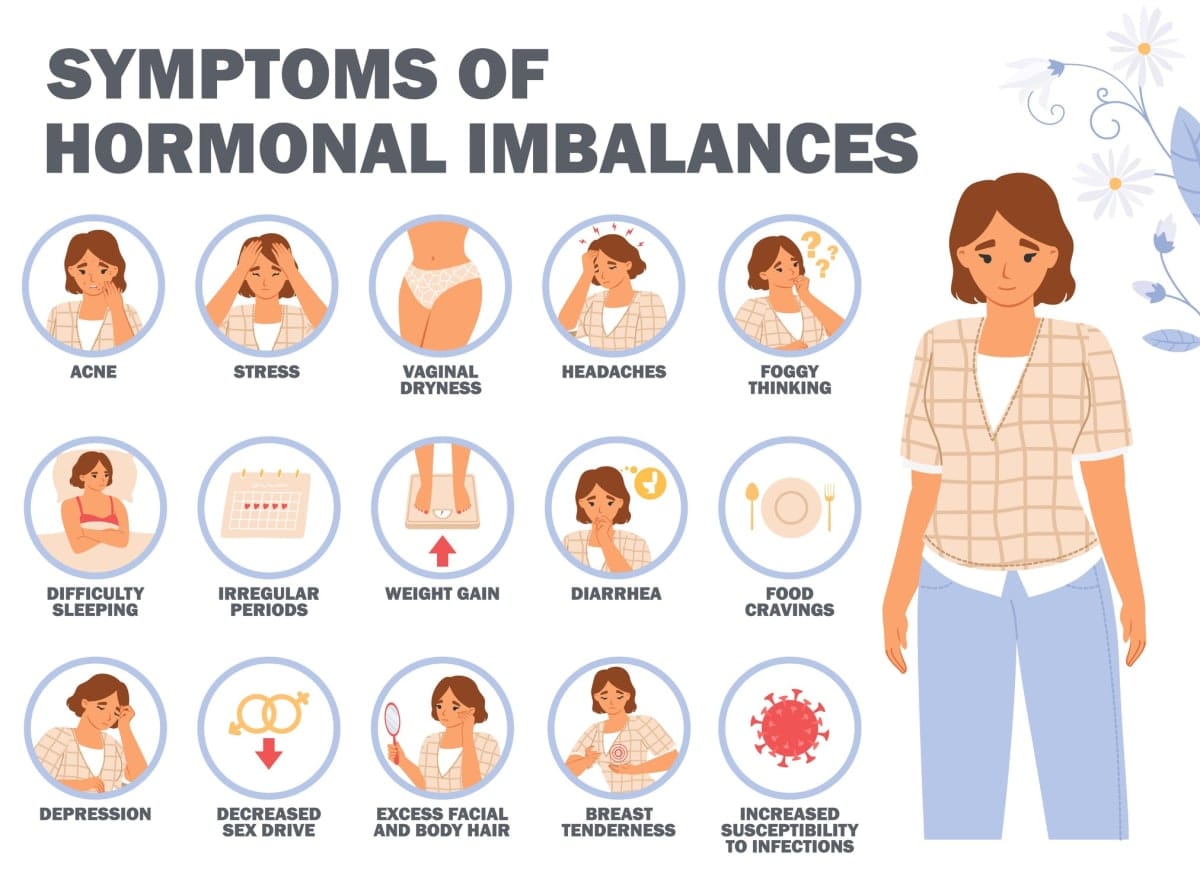
The hormonal and bodily changes experienced during menopause may lead to changes in eating behaviours, and how women feel about their bodies and overall sense of self.
As a result, menopause can increase the risk of the onset, redevelopment, or worsening of an eating disorder. Estimates suggest about 3.5% of people in the menopausal phase are also experiencing an eating disorder.
Eating disorders can commonly cause irregular or complete absence of menstrual periods, and low estrogen levels. So, it can be very difficult for women or people with ovaries with an eating disorder to understand where they are in the menopausal transition.
Shining a light on the menopause transition
It was this confusion that led Associate Professor Gemma Sharp and her team, including support from women’s health expert Professor Susan Davis, to develop a novel online resource to help explain the intersection of eating disorders and the menopausal transition.
“I noted a significant lack of education and support for women in midlife experiencing eating disorders,” she says.
“There’s so much attention on the risk in puberty of adolescence, but the other end of the reproductive phase, menopause, seems to have been forgotten.”
Read more: Women tell of devastation at early menopause diagnosis
Supported by a grant from the Australian Health Research Alliance, and in collaboration with Eating Disorders Victoria, Associate Professor Sharp and her team worked closely with women aged in their 30s in premenopause/perimenopause through to their 60s (postmenopause) in Australia who also had a lived experience of an eating disorder.
“When we started this project, we weren’t sure exactly what the end product would be. We listened to what women wanted, and tried to deliver on that,” she says.
It was very clear from the earliest stages of the project that the vast majority of the women had had traumatic experiences within the healthcare system.
They spoke of being dismissed by healthcare professionals for still having an eating disorder in midlife, and/or that their health practitioners only focused on the eating disorder, thus neglecting the women’s specific health needs and stage of life.
They also spoke of information and services always being focused on younger people with eating disorders, and that they felt overlooked. Furthermore, they mentioned their own lack of knowledge on the topic of menopause, with quite a few not being familiar with the term “perimenopause”.
They had a strong desire for more knowledge on the intersection of eating disorders and menopause. Thus, a novel online educational resource was born, was developed by women and for women.
While learning from health professional experts was important, learning from people with lived experience was considered equally, if not more, important.
The resource also provides information for supporting a loved one with an eating disorder in the menopausal transition, as well as brief information for health professionals.
As Associate Professor Sharp says:
“It’s wonderful to be able to create this resource. It’s an important step forward, but there’s a lot more work to do to better-support women in the menopausal transition with eating disorders, particularly with upskilling health professionals, and the creation of specific care services tailored for them.”
The menopause and eating disorders online resource is freely available from Eating Disorders Victoria’s website. The course contains detailed information, educational infographics, and a range of videos from people with a lived experience, as well as health professionals.
Associate Professor Sharp and her team are seeking feedback via the online resource to continue to improve the content and meet the needs of individuals accessing it.
Following this pioneering co-designed resource, Associate Professor Sharp and her team have created the international Consortium for Research in Eating Disorders (CoRe-ED), which brings together key voices in eating disorders research to improve treatment and care globally.
For further information, contact core-ed@monash.edu.





