Towards the end of her Monash University PhD 10 years ago, Associate Professor Jun Yang was asked to look into hospital guidelines for diagnosing a little-known but sometimes fatal condition that causes high blood pressure and therefore, potentially, strokes, heart attacks and kidney failure.
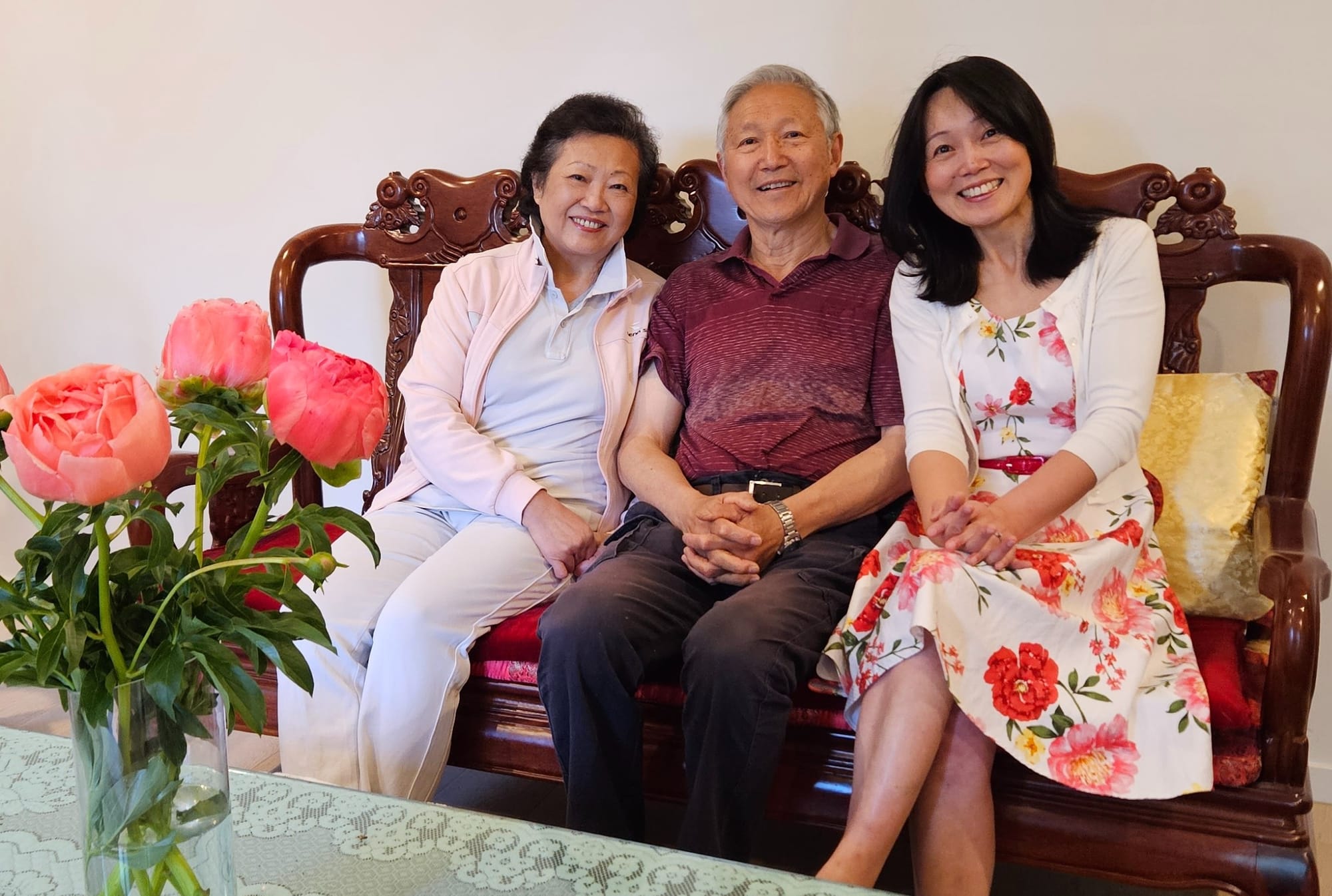
Little did she know the very condition she began to investigate would enter not only her life in an unexpected and very personal way, but also the lives of her father and mother – Monash University’s Professor Cherrie Zhu.
The condition is called primary aldosteronism (PA). Of the six million Australians with hypertension/high blood pressure, at least 10% have PA, yet the vast majority don’t know because it’s not usually tested for.
PA happens when a person’s adrenal glands (on top of the kidneys) produce too much of a hormone called aldosterone, which controls sodium and potassium balance in the blood. Excess aldosterone leads to high blood pressure, and also affects the heart, kidneys and blood vessels. It’s easily treated with medication, and some can be cured with surgery.
But according to Associate Professor Yang, a Monash Health endocrinologist, Monash University researcher, and head of the endocrine hypertension service at Hudson Institute of Medical Research, most doctors think it’s rare when in fact it’s not.
“The problem is once you say it’s rare in a textbook,” she says, “it takes many years to update textbooks. So, I think there are many health professionals out there who still have that old information in their brain.”
The condition was discovered in 1955. The root cause is likely to be a genetic mutation in an adrenal nodule or abnormal growth in both adrenal glands.
When Associate Professor Yang began working on the hospital guidelines 10 years ago, while finishing a doctorate on the aldosterone receptor, she saw the immediate problem of low testing rates. The single large hospital she was looking at only had a handful of patients diagnosed with the condition every year.
She thought about her own father, Lisheng Yang.

“He had high blood pressure which was never perfectly controlled,” she says. “He was taking four drugs for high blood pressure, and his GP would always tell him, ‘It’s OK. It goes up and down a bit, but overall, it’s OK.’”
She says “going up and down” is one of the indications for testing.
She tested him, and initially the test was normal.
“Then I realised all his medications could have caused false negative results. So I switched his medications around, and sure enough his results came back abnormal.”
She repeated the tests, then admitted her father for more specific testing in hospital, which confirmed his adrenal glands were making too much aldosterone and were resisting regulation. He then had another test to find out whether it was one or both adrenal glands causing the issue – it was both.
He went on an aldosterone-blocking tablet called Spironolactone as a targeted treatment, and is now fine, takes fewer pills daily (having stopped the previous four tablets), and pays a lot less for his medications.
Then, five years ago, her mother got it, too. She’s a professor of management at the Monash Business School, and also editor-in-chief of the journal of Chinese Management Studies.

“My husband had hypertension for many years,” she tells Lens. “His father died of a stroke. Then, one day at the GP, as a surprise – I am fit – my blood pressure was found to be very high. The GP prescribed a standard blood pressure-lowering medication to me. Two months later my blood pressure had gone up, so I changed medication again, and had three different ones in a year.
“Now my husband and I have exactly the same medication and we both have good blood pressure, and I have started to talk to everyone about hypertension and this problem. It seems that people don’t know this can be easily treated.”
Associate Professor Yang was surprised to find family affected, and had little idea the condition she researches would hit so close to home.
“It found me,” she says. “Having a personal motivation and personal experience always helps, because it made me realise how easy it is to miss this condition.”
Last year, Associate Professor Yang, Professor Grant Russell, Dr StellaMay Gwini, Professor Peter Fuller and PhD student Dr Renata Libianto led research published in the Medical Journal of Australia that called for nationwide screening and highlighted the central role of GPs in its early detection.
The team has now recruited GPs at primary care clinics for a randomised study across Victoria, South Australia and Tasmania that she hopes will eventually lead to screening all Australians with high blood pressure for the disease.
They’ve also set up PACE – the Primary Aldosteronism Centre of Research Excellence.
“We rarely get to cure a disease,” she says. “But there is a potential cure here.
“We have shown that if you offer people either the cure or targeted therapy, then they do better in the long term in terms of their heart health and kidney health. And yet, if you don’t recognise the condition, then not only do these people have worse and worse blood pressure, they also have much higher risk of stroke, heart disease and kidney disease.”