
Trial results of a new drug to treat Alzheimer’s disease, donanemab, shows it can slow cognitive decline by 35%. The drug has been hailed as a “turning point” in Alzheimer’s treatment.
"Turning point” in Alzheimer's fight as drug confirmed to slow the disease https://t.co/iSBuDS9NzL— BBC Breaking News (@BBCBreaking) July 17, 2023
But as usual, there’s more to the story. The study only included people with early or mild disease, not more advanced symptoms. Donanemab is not a cure for Alzheimer’s. Nor is it 100% safe.
So what did the trial actually find? And how might this drug affect the lives of people with Alzheimer’s disease?
Read more: New Alzheimer’s drug: What you need to know about donanemab’s promising trial results
What is Alzheimer’s disease?
There are more than 100 types of dementia, but Alzheimer’s disease is the most common, accounting for about 70% of cases.
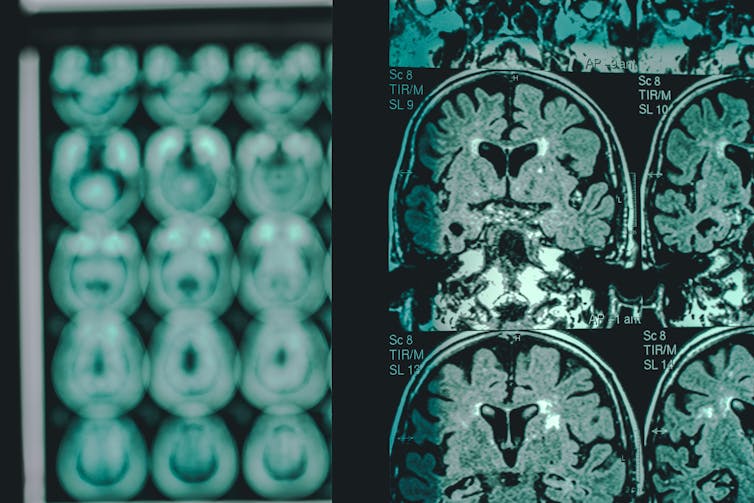
The disease is caused by the accumulation of two proteins, amyloid and tau. Amyloid can accumulate for at least 20 years before the onset of symptoms, forming clumps in the brain.
Once symptoms have started and are progressing, tau, a marker of cell damage, also begins to accumulate.
Clinical symptoms progress, on average, over seven to 10 years after diagnosis. But in Australia, there’s a lag of up to three years from the point at which people first develop symptoms before a diagnosis is typically made.
What have drug treatments aimed to do?
The “amyloid hypothesis”, which suggests amyloid is the key cause of the disease, has driven Alzheimer’s research for more than 25 years.
Multiple drugs targeting amyloid have, however, failed in clinical trials over most of that period, casting doubt on the validity of amyloid as a target – until recently.
Read more: What allegations of Alzheimer's research fraud mean for patients
Our bodies produce antibodies in response to the presence of a foreign invader such as a bacteria or virus. Mimicking the approach taken by our immune systems, scientists have developed antibodies in the lab that recognise amyloid as such an invader.
Specifically targeting amyloid, these drugs are known as monoclonal antibodies. Donanemab is one of three monoclonal antibodies targeting amyloid that have shown various degrees of success in clinical trials in slowing decline in people with early-stage disease.
OK, so what did the donanemab trial find?
The manufacturer’s clinical trial included 1736 patients with very mild memory loss due to Alzheimer’s disease, and with early clinical Alzheimer’s disease.
Half received donanemab by intravenous infusion over an 18-month study. The remainder were treated with a placebo (a “dummy” version).
The results were analysed by dividing the study population into two further groups – those with low to intermediate levels of tau, and those with high tau levels (high tau correlates with the presence of more advanced brain cell damage).
Those with low and intermediate tau declined by 35% less than those treated with placebo. About half of the treatment group cleared amyloid from their brains below the threshold used to diagnose the disease, over 12 months of treatment.
The high tau group did far less well.

Participants aged under 75 and those showing only mild cognitive impairment (rather than the full clinical picture of Alzheimer’s disease) had their progression slowed by about 50% over the same period.
Patients were assessed using both cognitive measures and measures of daily function, such as the ability to do personal and household tasks. The results translated into the treatment group showing levels of decline at 18 months that were experienced by the placebo group at 10.5 to 13.6 months, depending on the participant subgroup studied.
Important examples may be that they continue to be able to drive, pay bills, or attend activities outside of the home independently.
But both the treatment and the placebo groups declined overall. In other words, it doesn’t stop the decline, it slows it, in people with mild or early disease.
Read more: Lots of ‘breakthroughs’, still no cure. Do the new dementia drugs bring us any closer?
What are the downsides?
At least two patients in the trial died from complications of brain swelling caused by donanemab. About one-quarter of the treatment group showed some degree of swelling, most of which didn’t cause symptoms.
The cost of donanemab will be significant, at US$26,500, or about A$39,000 per year.
Donanemab has already been approved by the US Food and Drug Administration. Eli Lilly, the drug’s manufacturer, has applied to the Therapeutic Goods Administration (TGA) for approval for use in Australia.
But TGA approval is only the first step to making the drug available here. A further assessment will determine whether the Pharmaceutical Benefits Scheme subsidises the drug to make it affordable.
It’s likely any PBS listing would restrict the drug’s use to people whose disease state mirrors that of those included in the clinical trial population – people with early symptoms, who have had PET scans showing the presence of amyloid (and low and intermediate tau).
This is not a drug for everyone with Alzheimer’s disease.
Preparing for early detection and treatment
People have tended to delay seeking assessment of their memory symptoms because “nothing can be done anyway”. GPs may have been reluctant to refer to other specialists for assessment for the same reason.
The potential for early treatment means this needs to change. We also need to develop our diagnostic and treatment infrastructure (building the necessary PET scanners and infusion centres) that will be necessary to facilitate timely diagnosis and treatment when the drug does become available locally.
Read more: What is ‘sundowning’ and why does it happen to many people with dementia?

This article originally appeared on The Conversation.





