The recent decision by the federal government to reduce subsidised mental health sessions from 20 down to 10 has attracted criticism. While on face value this decision may appear to limit access to mental health care, it’s actually a step in the right direction towards equity-focused mental healthcare reform.
Australia’s mental health system is broken, costs $11 billion annually, and needs reform, says Graham Meadows, psychiatrist and Adjunct Professor in Monash University’s Faculty of Medicine, Nursing and Health Sciences.
“It currently better-serves the well-off, often failing to reach the groups who need it most,” he says.
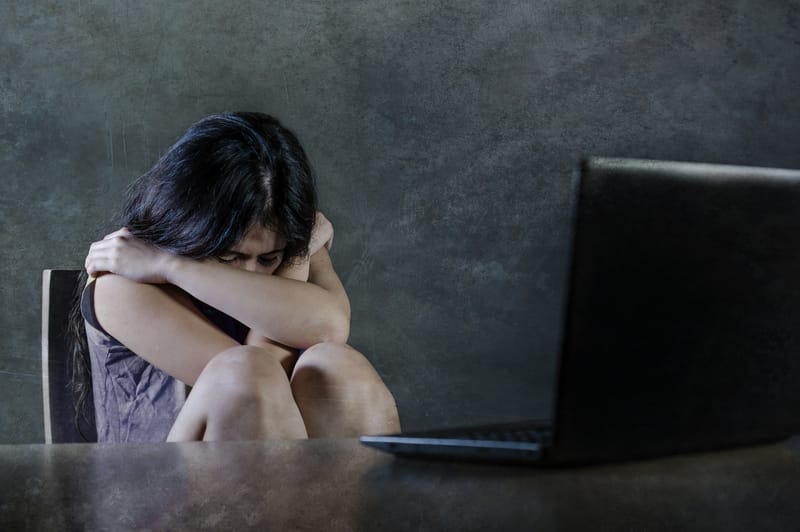
Women have the highest level of mental health distress in Australia
One of the largest groups missing out are women, particularly underserved women, who are the fastest-growing group reporting mental health distress.
We examined two decades of mental health data and found that gender and financial inequity are significant contributors to mental distress, with Australian women reporting poorer health and greater psychological distress than men.
Mental health distress in Australia has, since 2001, risen sharply in women aged between 55 and 64. While younger women reported the highest distress in all years since 2001, older women went from the lowest to the second-highest in 2018.
Very high levels of distress illustrate the effect of socioeconomic disadvantage even more starkly. For instance, 0.4% Australian men in the highest income quintile reported high levels of distress, while for women in the lowest quintile it’s 11.9%. That’s a 28-fold difference.
“Supporting women’s mental health will require much more than providing individual mental health services, regardless of the number of sessions.” says Dr Joanne Enticott, Senior Research Fellow with the Monash Centre for Health Research and Implementation.
“We need to deliver expanded and equity-focused health system reform, as well as addressing broader root causes of mental health distress.”
According to the World Health Organisation, these root causes include exposure to unfavourable social, economic, geopolitical and environmental circumstances – including poverty, violence, inequality, and environmental deprivation.
The role of financial inequity in mental health
We demonstrate that it will take 200 years for women to catch up to men in addressing the gender pay gap, and structural inequities in the superannuation system have yet to be addressed.
Women aged 50 to 65 represent the fastest-growing cohort entering homelessness, with one-third moving into older-age poverty.
Intersectional issues compound disadvantage and inequity for women, particularly those from culturally and linguistically diverse populations, and non-English-speaking backgrounds.
“Furthermore, women exposed to family violence are at greater risk of poorer mental health and, in turn, women with mental health issues are at higher risk of experiencing gender-based violence,” says Professor Megan Galbally, Professor of Psychiatry at Monash Health.
“Structural inequities then penalise women who have experienced and sought treatment for their mental health, including in the family court system.”

Women in family violence situations can also face barriers to accessing mental healthcare, including as a result of coercive control.
We assert that more broad structural reforms will be needed, in addition to accessible mental health services that understand the impact of gender-based violence on mental health, and are responsive to the needs of women.
“Psychological sessions, currently accessible to the more affluent in our community, will not help our most underserved women to put a meal on the table, pay the rent or necessarily escape gender-based violence,” says Professor Helena Teede, Professor of Research with the Monash Centre for Health Research and Implementation.
With the high prevalence of psychological distress and mental health disorders, population-level policies and strategies will be critical, alongside individual-level mental health services provided by a broader workforce and greater accessibility for the most underserved populations.
To ensure this occurs, we’ve proposed a National Institute for Equity and Women’s Health.
It’s time to understand the factors that influence health outcomes, and implement and evaluate evidence-based policy levers and structural reforms to reduce mental distress, as well as reforming mental health services.
The proposed institute will target those most in need, including women and those most financially insecure.