
It’s the mid-1990s, and Dr Anton Isaacs is at St John’s Medical College in Bangalore, India, thinking of specialising in surgery. He completes his medical degree and goes out to a rural hospital, assisting the resident surgeon, which he does for two years. But something isn’t right.
“Towards the end of my time there,” he says, “I woke up one morning with an insurmountable perception that surgery was not meant for me.”
Many years on, Dr Isaacs is with Monash University’s School of Rural Health, based in Warragul, still in health, but a long way from both Bangalore and surgery.
He’s currently researching COVID-19, as well as the implementation of “social prescription”, where GPs and primary health workers assess and help the individual as a whole.
But he’s just finished a mammoth two-decade body of work, over five published papers, which took him into the heart of vulnerable communities in Australia and India to try to address often deeply-hidden mental health problems.
A summary paper outlining the work is published in The Journal of Mental Health Policy and Economics.
But nearly 30 years ago, that nagging feeling isn’t budging, and Dr Isaacs knows he has to change paths – surgery isn’t for him. He quits thinking about surgery, and goes back to the drawing board, setting his sights on public health medicine.
He finishes in 2001, gets married and needs a job, so he asks the head of the college’s public health department if it’s true there’s an opening for a lecturer. There is, and he gets it, with one condition – he has to start a project on community mental health in a rural area outside the western edge of Bangalore.
“‘Sir,’ I say, ‘I have no idea about mental health and this rural area,’ Dr Isaacs says. “He says, ‘Do you want the job or not?’”

As it happens, a professor of community medicine and psychiatry at St John’s and a professor of psychiatry from Johns Hopkins University in the US have been promised US$250,000 by the Rotary Foundation (US) to set up a program looking at rural poor and their mental health.
But then, in September that year, terrorists fly aircraft into New York’s Twin Towers. Rotary Foundation’s head office is in one of the towers, and the project is postponed.
“In India,” Dr Isaacs says, “we have a lot of urban poor who live in slums, and we have rural poor who live in villages.”
“In India, we have a lot of urban poor who live in slums, and we have rural poor who live in villages.”
Rural people might be farmers, silk-makers, or do subsistence work with bricks. It’s estimated 20% of the country’s huge population suffers from a mental illness, while only 12% seek help. Rural Indians have poor access to healthcare, and poor knowledge of mental health conditions and treatments.
Rotary Foundation regroups after 9/11, but instead of US$250,000 for the stalled project, they donate $US25,000. That’s what they want Dr Isaacs to use to set up an as-yet-unplanned, uncoordinated, ambitious (and very local) project into a difficult and sensitive subject.
“I was told, ‘Just do whatever you can – it won’t be held against you if you do not achieve much’.”
He begins lecturing in public health medicine by day, and then, after work, goes to the hospital’s library to read.
“I was sitting there trying to figure out, ‘What do I do? How do I do this? What is the need?’ I had no idea whatsoever at that stage, but then I spent a lot of time reading up on the various models of mental health services, and the unmet need in rural areas and all that stuff. Then I decided, ‘OK, let’s give it a try. Let’s venture out.’”
The beginning of a 20-year journey
And so it begins in earnest – Dr Isaacs’ 20-year exploration of community-based systems to help the mental health of those least likely to be able to find it.
He’s authored five papers addressing the Indian experience in a village called Mugalur, near Bangalore, and also the Indigenous Australian experience in the Latrobe Valley, near Melbourne, in communities of the Gunaikurnai people.
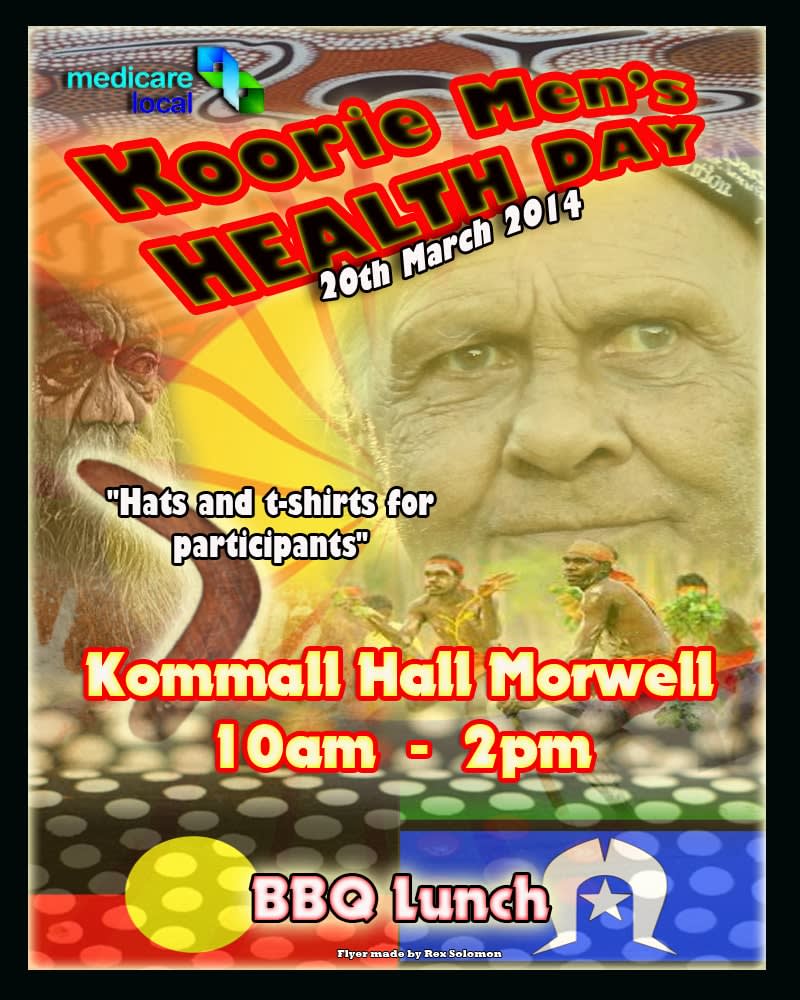
The summary paper (linked above) states that while the Indian service is still running, with more than 2000 registered “patients”, the Latrobe Valley model called the Koori Men’s Health Day, ran four times before running out of funding.
His two international case studies, the newest paper says, show “vastly different, albeit marginalised communities with an unmet need for mental health services”, with four “crucial elements” needed in delivering mental health care: mental health literacy, removing the stigma, cultural safety, and financial sustainability.
Starting from scratch
When the two-decade Indian study begins, there are no services in the area.
Dr Isaacs starts with a survey. He asks the hospital’s head of social work for help to find someone from the local area who could be trained to conduct surveys.
He hires four well-respected women from the community itself, who have completed high school but nothing further, to be paid community health workers. He then trains them to recognise mental health problems in people, and to conduct surveys. They get two motor scooters and go house to house.
“Anecdotal evidence indicated that carers of people with psychotic symptoms typically sought help from temples and Hindu priests,” the new paper says. “There were also no known satellite mental health services operating in the area. It was therefore assumed the mental health literacy among this population was low.”
The women go through 25 surrounding villages. They call themselves “Maanasi” workers. Maanasi in the local language, Kannada, means “woman with an intellectual mind”.
Weekly clinic visits to Mugalur
They survey 12,000 people in a year, by which time Dr Isaacs has a Bangalore psychiatrist, Dr Iby Neerakkal, who also subsequently moves to Australia, visiting a small community health centre and clinic in Mugalur once a week with a supply of pharmaceuticals for mental health disorders.
Even though local women know the four community health workers and speak to them about their issues, they’re initially silent in front of a male psychiatrist.
“They’re tongue-tied and not able to say anything, and just look down at her feet,” Dr Isaacs recalls. “Then the health worker steps in and says, ‘This is what has happened in her life’, and the psychiatrist looks at the woman and says, ‘Is that true?’, and the woman nods. So this worked out really well, because of all the stigma and all these issues associated with it, and then gender barriers.”
At first the medications are free or by donation – the team often gets bags of carrots or spinach.
It grows by word of mouth. By the third clinic, Dr Neerakkal has 30 patients to see during the course of an afternoon, which is too many for him, so the hospital in Bangalore puts its resident psychiatrists on a roster to visit the Mugalur clinic. It reaches 50 patients a day, all presenting with mental health issues.
“We heard about one woman who had schizophrenia in a neighbouring village, and she refused to leave the house, even though people were telling her to come and see us. She refused, and so our health workers went there and spoke to her husband, who had taken her to all the Hindu temples he could, but she wasn’t improving.
“Finally, I went to his house, sat with him and said, ‘I’ll make you a deal. You allow us to take your wife to the hospital, we will give her free treatment. You don't have to pay for anything, and we will bring her back in our Jeep, and if she does not improve, then we will not trouble you again.’”
A few days later, the husband visits, and his wife sits up in bed eating and chatting. She goes home two weeks later.
“He was so touched. He said, ‘Do you know what a big difference you have made? I have not been able to speak with my wife like this for 13 or 14 years.’ We became like demigods, because we were creating miracles in that place.”
A local Muslim family, a minority in the area, seek help for their young adult daughter who sleeps and cries all day. She’s given medication for depression and is able to resume her life within her family, and soon gets married.
The success stories continue, but eventually the money runs out. A local Rotary club steps in to continue the funding.
Reaching out for collaborators
Dr Isaacs begins to look further afield. He reads an article by then-Monash University researcher Professor Fiona Judd, who’s now with the University of Melbourne, about rural mental health, and he writes to her, in 2006, asking to collaborate.
Some months later he gets an email from the School of Rural Health and finds himself being interviewed by one of its then-directors, Professor Mark Oakley-Browne, who tells him he could get scholarships if he wants to do a PhD at Monash, in Gippsland.
“I told my wife, ‘This is the situation, what do you think?’ She said, ‘I think you should go for it. Do you know the first thing you told me when we first met? That you would like to do a PhD, preferably from an international university.’
“I wasn’t keen. I was not keen to leave my wife and son. My son was one-and-a-half years old. She said, ‘No, you must get back to him, find out what this is all about. Let’s do this.’”
Dr Isaacs wins entry to Monash University to undertake a PhD in rural mental health with two scholarships. His then-pregnant wife and child move in with her parents in India. They sell possessions, and Dr Isaacs comes to country Victoria on his own to begin. His family join him later, when he and the newest project are up and running.
“I had to ask my in-laws to look after my wife and children,” he says. “I said, ‘I have no money to give you to look after them.’ And my father-in-law said, ‘Don't worry. Just go and do what you have to do.’”
The project is mental health in Indigenous communities around Morwell and Moe.
“The only Aboriginal Australian I knew about at the time was Cathy Freeman,” he says. “People were saying I was mad, no idea about First Nations issues, no idea about Aboriginal people, ‘You won’t finish this PhD, I don’t know who brought you here.’”
“The only Aboriginal Australian I knew about at the time was Cathy Freeman,” he says. “People were saying I was mad, no idea about First Nations issues, no idea about Aboriginal people, ‘You won’t finish this PhD, I don’t know who brought you here.’”
This troubles Dr Isaacs. Maybe his doubters are right, and he isn’t the man for the job; he won’t be able to do it justice. The cultural gap is wide.
He meets Monash’s Adjunct Professor Marlene Drysdale, a senior Aboriginal health educator now working with Eastern Victoria GP Training.
She becomes his bridge over the divide. She introduces him to colleagues specialising in Indigenous health, and he begins a long immersion into local communities – “all the celebrations, meeting cultural advisors, going to communities. It was a very steep learning curve,” he says.
This time, the project is with men. “I had to spend time building rapport. They had to trust me, because I was this new bloke from a foreign country. It took about two years to build their trust.”
He spends time talking and asking questions about mental health issues, and offering men retail vouchers in return for their time.
He knows from the data that Aboriginal men are over-represented in more severe forms of mental illness, and also over-represented in patient care, and that they find it hard to seek help and tend to leave it until crisis point.
Men tell him of “lack of trust in the health service, fear of hospitals, long waiting times, gender mismatches with caregivers, cultural differences and racism … the stigma of being labelled with a mental illness is particularly severe among those who experience economic disadvantage and face multiple stigmas [already].”

Dr Isaacs ends up winning funding from Beyond Blue for his Koori Men’s Health Days in Gippsland’s Latrobe Valley. The days are designed and run by local men, which encourages them to tell all their friends and family.
Mental health services at one of the local hospitals become involved. The days – for local Indigenous men over 18 – are billed as “health days” rather than mental health days. Participants can get their blood pressure, diabetes and hearts checked, as well as any mental health issues.
The venue is chosen by local Indigenous stakeholders, who also organise transport. Healthy food is provided at the venue.
Problems are identified regarding men’s isolation and separation from family, as well as issues with literacy and numeracy that the participants say makes them feel ashamed and less likely to get a job or see friends and family, leading to poorer social and emotional wellbeing.
The days are successful and valuable, but then the funding dries up and they’re discontinued. Alternative funding couldn’t be found, and the Koori Men’s Health Days no longer run, and Dr Isaacs can no longer gather data from them.
“The needs are a lot more with Victorian Aboriginal people because the issues and the barriers are far, far more. There are lots of political issues. There are lots of cultural issues,” he says.
Near the end of the run of annual Koori Men’s Health Days, there’s a public webinar.
“We had cultural consultants online who are all Aboriginal men, respected in the local community, and myself, and we were talking about all these issues.
“The facilitator asked one of them, ‘What do you think? Now that you have discussed all this, what do you think you would like to do next?’ And they said, ‘Whatever Anton wants to do, we will do.’
“I was really embarrassed on the one hand, and on the other hand, I thought, ‘Wow. That's kind, because that's the amount of trust that we were able to build. They knew surely that whatever I do, I would do only for their betterment and for their community.”





