
Whether it’s debilitating periods or depression during menopause, women with mental health problems are told to grin and bear it as their crushing emotions are “simply nature taking its course”.
But what we now know, and science has told us, is that many women of all ages are living with mental illnesses that may be related to female hormones and/or other unique parts of their biology.
A woman can experience pre-menstrual or menopause-related depression that’s as serious as any other type of depression.
Yet it can be easily written off as part of a “normal” hormonal cycle. At its worst, such conditions can lead to serious mental illness or even suicide, without the true cause being identified.
This is a national – and international – tragedy.
A woman can experience pre-menstrual or menopause-related depression that’s as serious as any other type of depression.

More awareness needed
While a growing body of research is focusing on these and other important aspects of women’s mental health, we need much more, and public awareness needs to improve.
Unfortunately, women experience nearly twice as much depression as men, four times as much anxiety, and 12 times the rate of eating disorders.
Mental illness for women also involves a complex interaction of biological, psychological, and social factors. This means that the causes of, and best treatments for, conditions such as depression, anxiety, trauma disorders, addictions, and self-harm are different compared with men.
Environmental factors that impact many women, and can contribute to mental ill health, include being subjected to violence, having less power, lower wages, and struggling with negative cultural expectations.
If we better-recognise and treat these conditions, life will improve for the women affected and their families. They need to know that, in many cases, they shouldn’t have to suffer unnecessarily.
These conditions are real
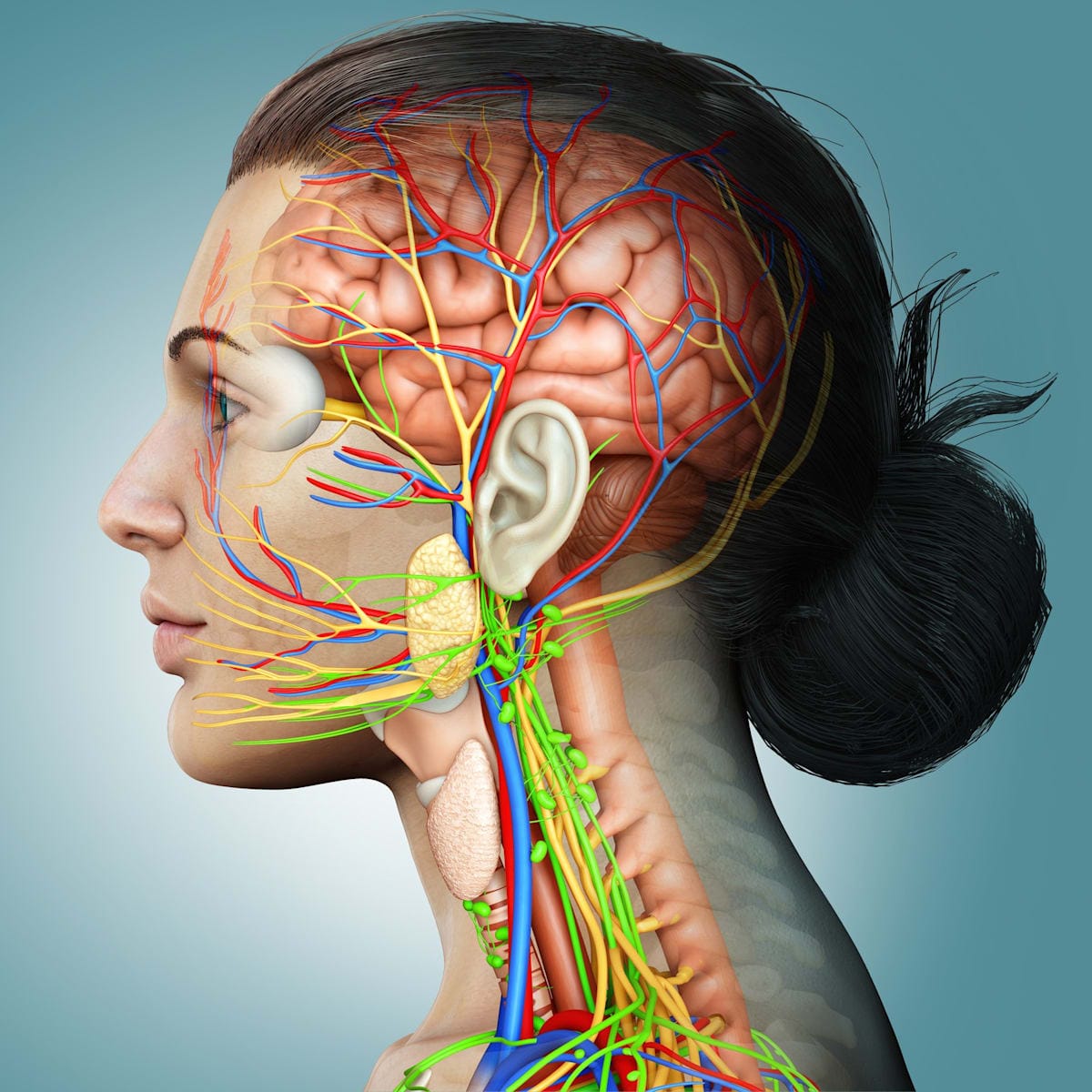
To understand mental illness, we must understand neurobiology, which is the way nervous system cells are organised into functional circuits that process information and mediate behaviour.
If something goes wrong with these circuits, whether it’s caused by genetic, hormonal, environmental, or a combination of factors, mental illness can result.
For this reason, we need to focus on the physiology of the brain as well as psychological and environmental factors. We call this a biopsychosocial model – one that considers a range of factors.
This model is also important when looking at mental illness caused by trauma, which is a major issue for women, particularly those physically, sexually or emotionally abused as children and/or subject to family violence.
Some will develop complex post-traumatic stress disorder, which may be undiagnosed or labelled borderline personality disorder, which is marked by dysfunctional and sometimes erratic behaviour.
Until we identify and acknowledge the cause of these conditions, properly define them as mental illnesses and improve their treatment, too many women will continue to suffer.
Improving research and treatment
After more than 30 years of Monash University-led research in this under-recognised field through the Alfred Hospital’s Monash Alfred Psychiatry research centre (MAPrc), we’re finally on the cusp of real change.
We envisioned and drove the establishment of Cabrini Women’s Mental Health Hospital, Australia’s first women’s-only mental health hospital.
We’re now officially launching HER Centre Australia, which has a revolutionary approach to women’s mental health through a model encompassing health, education, research, and public advocacy.
Unlike most other centres, HER Centre’s team of health professionals and researchers is committed to developing world-first tailored treatments and interventions for women. We’re committed to being leaders in women’s mental health.
Research is conducted in clinical trials for women – which means the results can be quickly translated into new medications and programs.
Making a difference
Among other things, we’re working on hormone-based treatments for women with menopausal depression. This isn’t just “change of life grumpiness”, it’s a potentially serious illness.
We’re conducting clinical trials with new forms of oestrogen and treating women, while educating health professionals about the need for tailored hormone treatments for women.
Despite this, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) still has no definitive condition called menopausal depression.

There is very poor understanding of this illness, which often gets diagnosed as bipolar disorder. We also need to better-understand pre and antenatal depression, which affects many women.
HER Centre will cover a wide range of conditions affecting women, including bipolar disorder, body dysmorphic disorder, complex post-traumatic stress disorder, eating disorders, family violence, depression, postpartum depression, and schizophrenia/psychosis.
It will be at the forefront of new treatments such as cannabis oil, if they’re proven to be effective. It will also offer courses for health professionals, such as psychiatrists and GPs, to help them better-understand the likes of period and menopause depression.
Eating disorders are another condition that requires more of a neurobiology focus, while exploring and acknowledging environmental factors such as social media and peer pressure.
A national health priority
To improve the situation, it needs to be more widely recognised that hormones aren’t just about the ovaries and the uterus. They’re very potent in the brain.
Just as violence against women has attained the spotlight it deserves through the bravery of women such as Grace Tame and Brittany Higgins, we need to shine a light on women’s mental health.
Trauma can play a significant role in mental illness, and knowledge about this is power.
For this and other reasons outlined, women’s mental wellbeing must be a national priority.
We need a national conversation that champions change in health systems and society generally. If we can better-identify and treat these often-hidden conditions, we’ll all be better off.





