
The sudden and unexpected appearance of the monkeypox virus in countries not endemic to the disease has the world's medical community on high alert.
Since 13 May, and as of 2 June, there have been 780 laboratory-confirmed cases of the disease reported to the World Health Organisation, from 27 member states. This compares to just 92 cases in 12 member states up to 21 May.
Non-endemic countries where the disease has been reported include Australia, Belgium, Canada, France, Germany, Netherlands, Portugal, Italy, Spain, Sweden, United Kingdom and the United States.
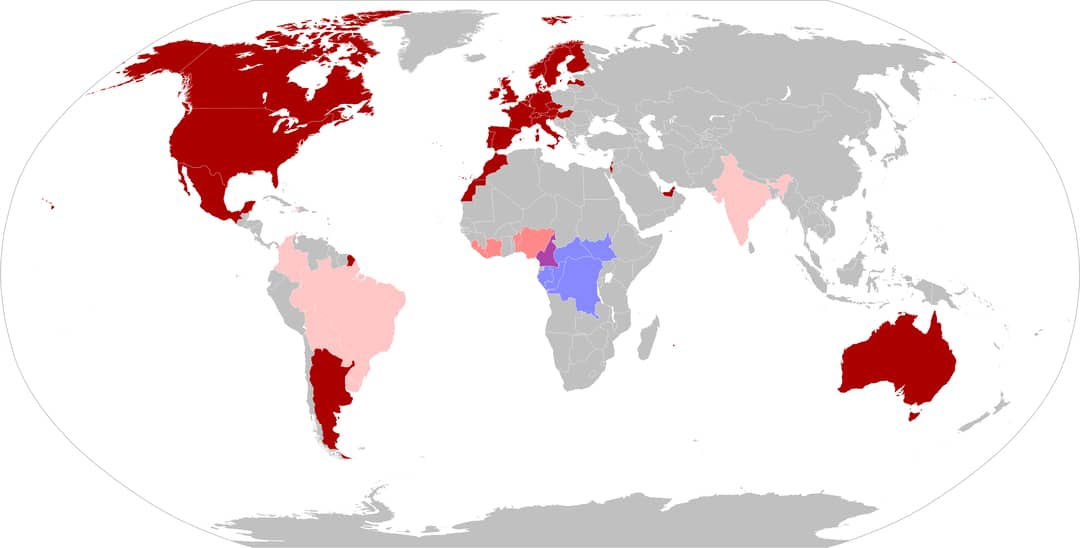
The first human case of monkeypox was recorded in 1970 in the Democratic Republic of Congo, and is a viral disease that occurs mostly in central and western Africa.
As the situation evolves, WHO expects more cases of monkeypox will be identified as surveillance expands in non-endemic countries. So far, there have been no deaths associated with this outbreak.
UK records 77 more cases of monkeypox, taking total to 302https://t.co/vdDRX2kQBE
Contacts of confirmed or suspected cases who develop rash with blisters asked to contact sexual health clinic— Reiner Grißhammer (@erlesen) June 7, 2022
What is monkeypox?
Monkeypox is a zoonotic disease caused by an orthopoxvirus that results in a smallpox-like disease in humans.
The disease is named monkeypox because researchers first detected it in laboratory monkeys in 1958.
The virus is believed to transmit from wild animals, such as rodents, to humans – or between infected people.
A few thousand cases occur in Africa yearly, typically in the western and central parts of the continent. Up to now, cases outside Africa have been limited to a handful associated with travel to Africa or the importation of infected animals.
The number of cases detected outside Africa has already surpassed the number detected outside the continent since 1970, when the virus was first identified as causing disease in humans. This rapid spread is what has scientists on high alert.
What are the symptoms?
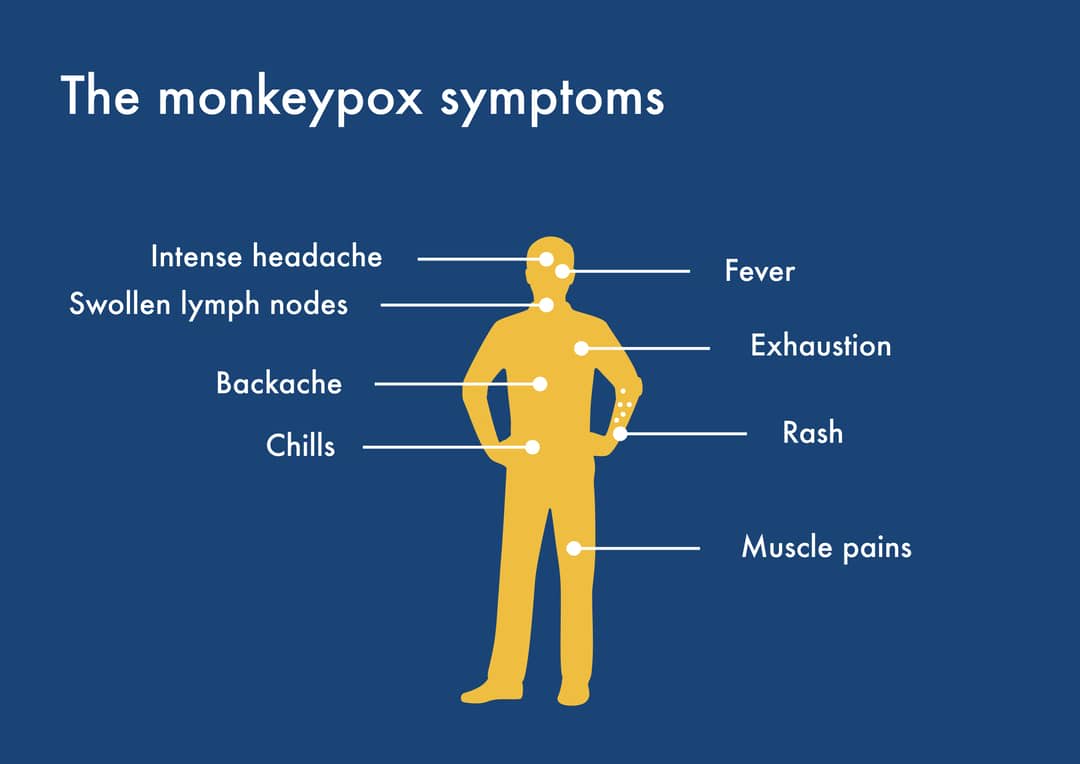
Monkeypox typically presents with fever, rash and swollen lymph nodes, and may lead to a range of medical complications. It’s usually a self-limited disease, with symptoms lasting two to four weeks.
Severe cases can occur. The case fatality ratio is between 3-6%.
Re-emergence of monkeypox
The resurgence in monkeypox cases is being attributed to waning immunity, although deforestation may also be a factor, or can even act in potentiation.
Monkeypox virus, variola virus (smallpox), and vaccinia virus (smallpox vaccination) are closely related to orthopoxviruses. At the time when smallpox was rampant, no cases of monkeypox were reported. This could be attributed to the focus on smallpox, and the fact the presentation of the two diseases are similar, or that the lack of laboratory confirmation of the etiologic agent led to an assumption of smallpox.
Historical data shows that smallpox vaccination was approximately 85% protective against monkeypox.
Smallpox was eradicated by vaccination in 1980, and the vaccine phased out. But because it also protects against monkeypox, the winding down of vaccination campaigns is another potential reason for the jump in monkeypox cases.
What are the possibilities of a new virulent strain of monkeypox?
We still don't have much data on this. The fact that so many cases are being reported in multiple countries certainly suggests that this strain is more transmissible than others.
We still need to look at the current genomic data on the circulating strain to know more. One thing for certain is that the threat posed by this virus should not be taken lightly, and increased surveillance and vigilance is needed.
But unlike SARS-CoV-2, which spreads through tiny airborne droplets called aerosols, monkeypox is thought to spread from close contact with bodily fluids, such as saliva from coughing.
This means a person with monkeypox is likely to infect far fewer close contacts than someone with SARS-CoV-2, says Jay Hooper, a virologist at the US Army Medical Research Institute of Infectious Diseases.
Both viruses can cause flu-like symptoms, but monkeypox also triggers enlarged lymph nodes and, eventually, distinctive fluid-filled lesions on the face, hands and feet. Most people recover from monkeypox in a few weeks without treatment.
Researchers in Portugal recently uploaded the first genomic draft of monkeypox from the recent outbreak. Preliminary genetic data shows that the virus is related to a viral strain predominantly found in western Africa. This strain causes milder disease and has a lower death rate – about 1% in poor, rural populations – compared with the one circulating in central Africa.
But exactly how much the strain causing the current outbreaks differs from the one in western Africa – and whether the viruses popping up in various countries are linked to one another – remains unknown.





