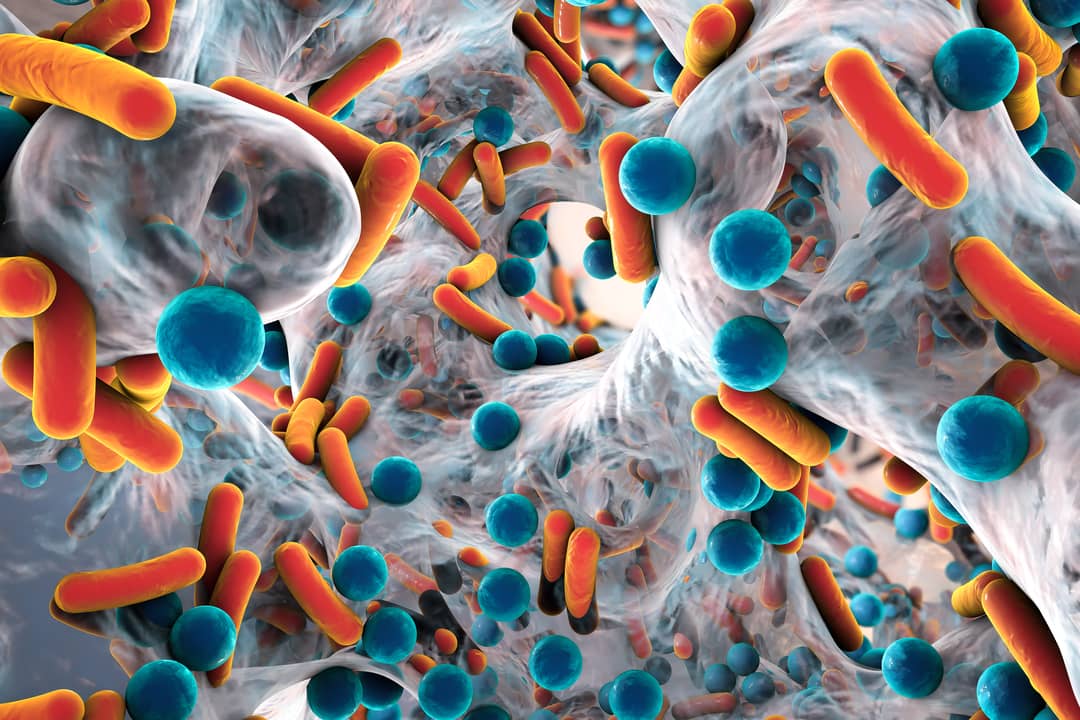
Bacteria can be found almost everywhere, from inside our gut to extreme environments such as Antarctica. While not all bacteria are harmful to humans, a handful can cause severe human infections that can be potentially fatal.
Since the discovery of antibiotics in the 1950s, bacterial infections have been successfully treated using these powerful drugs. Antibiotics work by either killing the bacteria directly, or blocking its ability to grow and multiply.
But due to overuse and a lack of regulation in many countries, many bacteria are now resistant to antibiotics.
These antibiotic-resistant bacteria, also known as superbugs, cause 700,000 deaths annually.
The saying “What doesn’t kill you makes you stronger” holds very true in the bacterial world. When survival is at stake, bacteria can mutate their DNA quickly to adapt to any stress, including antibiotics. This ability helps them develop new mutations that allow them to resist even the latest antibiotics.
To complicate matters, they can even share these antibiotic-resistant DNA materials with bacteria that were not previously resistant.
Unfortunately, the current antibiotics discovery and development pipeline has been running dry the past 20 years, because it takes 10 to 15 years and more than US$1 billion to develop new antibiotics.
On the other hand, bacteria can render new antibiotics that take years to develop to become ineffective in a few months. Hence, this field isn’t attractive or sustainable for pharmaceutical companies, with some even moving away from antibiotic development in recent years.
What can we do to slow the rapid rise of superbugs?
Although careful antibiotic use should be the main thrust to prolong their usefulness, we need to also come up with new strategies to treat superbugs.
My research aims to discover new anti-virulence treatment targets in bacteria that don’t trigger their “survival response”. We also hope to develop an alternative anti-virulence agent that can be rapidly and easily modified to counter new bacteria mutations.
It’s almost impossible to stop bacteria from developing mutations against antimicrobial agents once their survival is threatened. Therefore, I’ve been advocating for anti-virulence strategies rather than “anti-survival” strategies employed by the current generation of antibiotics.
Read more: Thermobifida fusca: the manure-dwelling 'hot bug' that may result in life-saving antibiotics
Anti-virulence strategies aim to disarm the bacteria without directly killing them, and thus reduce the possibility of developing mutations. They will no longer cause infection and be cleared naturally by the immune system or with currently available antibiotics.
Current antibiotics have been discovered by screening massive compounds produced by soil bacteria, fungi, and plants. These compounds tend to have very distinct chemical structures and might be challenging to modify. Hence, instead of joining the bandwagon of discovering antibiotics from the environment, we decided to screen for functional nucleic acids such as aptamers and catalytic DNA/RNA.
This nucleic acid group is particularly attractive, as it’s well-characterised and easily adjustable with a known predicted outcome. To shorten the time taken to develop these anti-virulence drugs, we aim to develop modular functional nucleic-acid based therapeutics as an alternative that are robust and amendable in a short time if resistance does develop.
Read more: Taking the superbug fight to nursing homes
My team is investigating whether we can disable the ability of bacteria to cause infection using our robust anti-virulence nucleic-acid discovery pipeline to slow the development of resistant bacteria.
My group has experience working with functional nucleic acids, and a good understanding of the molecular aspect of bacterial pathogenesis of many harmful bacteria, including the crucial ESKAPE pathogens.

We have the facility to test our approach and the practicality of our discovery pipeline. We’ve also established an insect-based infection model to allow rapid and massive parallel screening of these agents in an in vivo-like environment to discover promising candidates.
Hence, we seek to combine the modularity of functional nucleic acid and anti-virulence strategy to address the antimicrobial resistance challenge.
This research aligns with Monash’s Impact 2030 strategy plan, addressing global challenges under the “Thriving Communities” theme, and the School of Science focus areas in health sciences.
Our hope is that this research will provide a sustainable antimicrobial drug discovery pipeline proof-of-concept, and shortlist some promising anti-virulence candidates for clinical trials.
We hope the results of this project will inspire more research groups and pharmaceutical companies to remain hopeful about the discovery of alternative antimicrobials.
With the right strategy and perseverance, we can slow the rapid rise of superbugs and prevent the return of the pre-antibiotics era before the 1940s, where even a small paper-cut infection could be life-threatening.





