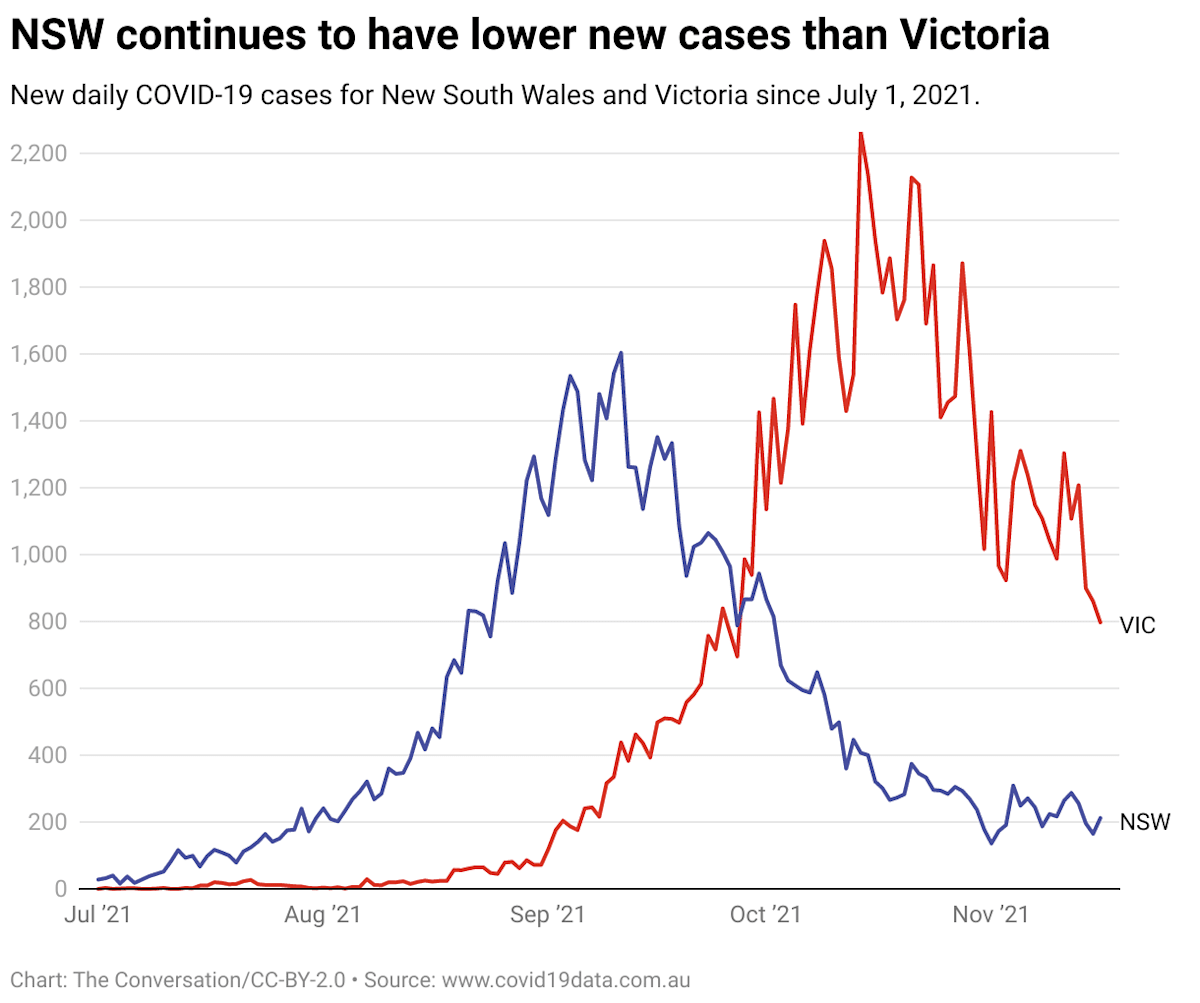
New daily COVID cases in New South Wales decreased rapidly from a peak of more than 1600 in early September, and are now hovering at about 200-250 new cases per day.
They’ve remained low even since lockdown restrictions were eased on 11 October.
By contrast, new daily cases in Victoria have dropped from a peak of more than 2200 on 13 October to plateau around 1000 – though they’ve dropped a little further to about 800 in the past few days.
So how come NSW’s cases dropped so much quicker and further than Victoria’s?
The easy answer is that it’s all just luck, good or bad. But if we look hard enough, we can usually find reasons that are likely to provide at least some of the explanation.
Overwhelmed contact tracing and lockdown fatigue affected both states, so it’s unlikely either of these accounted for a major part of the difference between the states’ cases.
It’s more likely structural factors are playing a major role in driving Australia’s diverse epidemic. These include climate and the connectedness of populations.
Read more: Why has Victoria struggled more than NSW with COVID? To a demographer, they're not that different
Both states’ COVID waves had similarities
The COVID outbreaks in NSW and Victoria had several similarities. Both quickly took root in the suburbs of each state’s capital city with higher population densities and proportions of essential workers.
These regions were also generally younger, and so had lower vaccine coverage because our vaccination policy was to gradually progress from older to younger ages.
As the outbreaks spread across both states, populations with lower coverage were often the most severely affected, with outbreaks often affecting suburbs and towns with lagging vaccination rates.
Does anyone have a good theory on why Victorian Numbers aren’t dropping faster despite high vax rate? Perhaps more testing ? But I’m a bit surprised https://t.co/U1fSlOR2C8— Samantha Maiden (@samanthamaiden) October 21, 2021
There were also important differences. Sydney’s wave started earlier, when the national rollout was less advanced. But targeted vaccination of high-risk suburbs was key to stabilising case numbers.
Strict lockdown measures were implemented earlier in the course of the epidemic in Victoria, and yet were insufficient to achieve a quick return to elimination.
Although contact tracing in NSW has previously been lauded as the country’s “gold-standard”, the effectiveness of any state’s contact tracing rapidly declines as daily case numbers rise through the hundreds. So, differences between the states’ contact tracing is a less likely explanation for the differences in case numbers.
Similarly, lockdown fatigue was a factor in both states. Melbourne has spent more days locked down in total, but Sydney’s recent lockdown had started earlier.
Ultimately, both epidemics were controlled through vaccination. Although this has involved both carrot and stick, this can nevertheless be attributed to unprecedented engagement by the public in the vaccination program. Australians have shown how highly motivated they are to get vaccinated once the supply issues were finally resolved, with obvious payoffs.
So, it’s hard to find a single reason for why the outbreaks played out differently in the two states. While there are several similarities between the two cities’ epidemics, there are also differences, which push in both directions.
Read more: Mapping COVID-19 spread in Melbourne shows link to job types and ability to stay home
Weather seems to be involved
In Australia and elsewhere, scientists have frequently proposed climatic factors as one explanation for markedly different COVID waves across the world.
This has been difficult to fully define; there are exceptions to any rule, and several analyses have suggested no effect.
Nevertheless, the following factors appear to make COVID outbreaks harder to control:
- Higher population density
- Higher latitude
- Colder and drier weather.
Since the first explosive epidemics of 2020 in Europe and North America, major high-income cities in winter in temperate regions have often been hit the hardest. For example, New York, Paris and London.
This is consistent with the cyclical pattern of non-COVID coronaviruses, which are responsible for large waves of common cold symptoms each winter.
Several respiratory infections appear to transmit more efficiently in cold, dry climates.
Research shows coronavirus thrives in dry air (and August is coastal Australia's least humid month) https://t.co/km3hldIORQ via @ConversationEDU For Every 1% decrease in relative humidity, it seems cases increase by 7-8%. They saw no correlation w temperature/windspeed/rainfall.— Sagar (@VidyasagarLab) August 18, 2020
This international pattern appears to have played out similarly in Australia.
Melbourne is a significantly colder and drier city than Sydney, and has needed more restrictions than Sydney to achieve control of COVID. Sydney is colder and drier than Brisbane, and similarly needed more restrictions to gain control.
There are biological reasons why respiratory viruses might transmit more efficiently in cold weather. However, given the importance of indoor transmission to COVID, human behaviour and where we choose to associate at different times of the year may be much of the explanation.
Outside of our major cities on the eastern seaboard, population density and connectedness are likely the dominant factors.
Although we don’t fully understand the contribution of each of these elements, it seems clear structural factors, such as population density, city size, socioeconomic status and climate are crucial to how COVID spreads.
We now know vaccination doesn’t just protect against disease and death, but also has a substantial effect on transmission – such that we have the ability to slow COVID outbreaks without necessarily resorting to lockdown.
How will COVID spread in Australia going forward?
In our wide, diverse land, we’ll inevitably continue to see different COVID outbreaks in different regions.
Our large cities will likely remain at, or close to, herd immunity through some combination of transmission and vaccination.
Outbreaks will likely occur sporadically in remote areas less connected to major urban centres. Such rural and remote regions may go for months without cases, even with moderate vaccination coverage. However, outbreaks will occur in these communities, particularly as vaccine-induced immunity wanes and long periods without cases lead to complacency about the need for vaccination.

This article originally appeared on The Conversation.