Just as sharing similar life experiences with another person can be unifying, the same can be said for individuals with chronic diseases or health conditions.
While access to healthcare professionals is crucial, having a peer who shares the same or similar condition could serve as a great source of support in a person’s journey towards becoming a healthier version of themselves.
Last year, the Department of Statistics Malaysia said heart attacks remain the leading cause of death in Malaysia. Diabetes is also a major concern in the country, with seven million Malaysians projected to have the disease by 2025.
Metabolic syndrome affects up to 43.4 per cent of the Malaysian population. This is in stark contrast to the country’s neighbour, Singapore (26 per cent). Despite this, data on metabolic syndrome within the Malaysian context is still scarce.
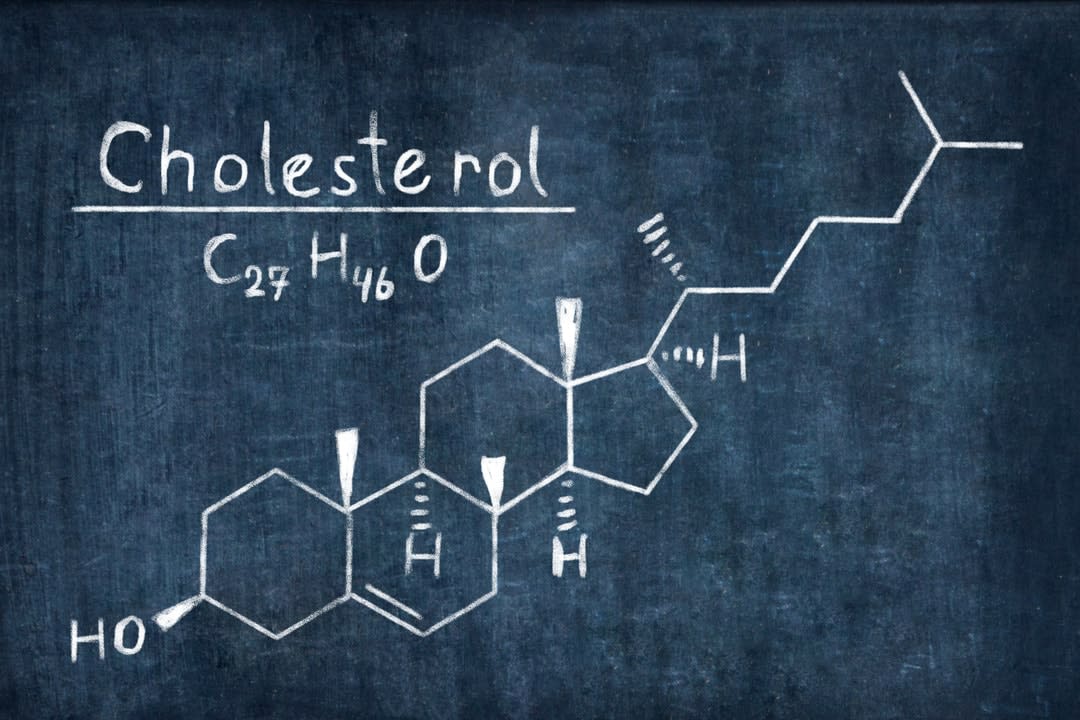
What is metabolic syndrome?
Metabolic syndrome is a cluster of disorders that can increase an individual's risk of developing type 2 diabetes mellitus and cardiovascular diseases. The disorders include high blood pressure, high triglyceride levels and blood glucose levels, low HDL cholesterol (or "good" cholesterol), and abdominal obesity.

Studies have shown that lifestyle modifications can be a better option than medications for long-term prevention of metabolic disorders such as diabetes. However, there's growing evidence that by integrating a peer support framework, individuals with chronic diseases can improve outcomes.
Researchers at Monash University Malaysia are trying to further understand this issue.
The Malaysian context
Various lifestyle factors influence metabolic syndrome, says Dr Amutha Ramadas, a senior lecturer at Monash University Malaysia's Jeffrey Cheah School of Medicine and Health Sciences.
These include sedentary lifestyle, physical inactivity, poor sleeping patterns, smoking, and alcohol consumption.
Dietary habits such as the speed of eating, how often one eats out, skipping breakfast, and late dinners are also associated with an increased incidence of metabolic syndrome.
Despite the availability of such data, there's still a limited understanding of the condition within the Malaysian context. A previous study describing the association between physical activity and metabolic syndrome was conducted 13 years ago, with more than 8000 participants.
But Dr Amutha, along with five other researchers from the University, is hoping to shed more light on this situation.
Last year, the team investigated the association of various sociodemographic characteristics, lifestyle factors, and diet habits with metabolic syndrome among Malaysia's three major ethnic communities.
Their cross-sectional study – carried out in two phases – took place in the country's southernmost state, Johor. Based on their sample of 481 Malaysians aged 18 and over, metabolic syndrome was found in 32 per cent of the group. A sub-analysis revealed a glaring difference between the three major ethnicities. Indians recorded the highest rate of metabolic syndrome (51.9 per cent), followed by the Malays (36.7 per cent), and the Chinese (20.2 per cent).
Dr Amutha said the data reaffirmed that low physical activity increases one's odds of developing metabolic syndrome by at least four times, while eating quickly can double the odds of metabolic syndrome.
"Despite this, sadly, we are certainly lacking in making effective lifestyle changes to prevent metabolic syndrome, or to improve the condition,” she says. “By the time we seek help, it's often too late for lifestyle changes alone to make a difference, and we have to resort to drug therapy."
Tapping into the power of peer support
As metabolic syndrome is a lifestyle-associated condition, lifestyle behaviours have to be the first line of approach towards the prevention and management of the disease, explains Dr Amutha.
The National Cholesterol Education Program Adult Treatment Panel III recommends lifestyle modification as the first strategy in the management of metabolic syndrome – a sentiment also echoed by the Malaysian National Non-communicable Diseases Planning 2010-2015.
However, the number of such interventions in Malaysia is limited. Past studies have shown that peer support interventions can benefit adults with certain chronic conditions, but there's limited evidence on its feasibility and effectiveness among people with metabolic syndrome.
Peer support is a non-hierarchical and mutually beneficial relationship with others who face the same health problem, and has been used in group-based lifestyle interventions evaluated in the general population.
As such, the Monash University team created "PERSUADE" (PEeR SUpport program for ADults with mEtabolic syndrome), an evidence-based and community-specific nutrition and lifestyle behaviour support program. Participants were divided into four groups according to their location, while one peer leader was appointed for each group, and trained to deliver the PERSUADE peer module.
Forty-eight community members with a median age of 46 were involved in the peer program, held over a 12-week trial period last year.
Participants were assessed before and after the trial, while weekly measuring sessions that tracked figures such as participants’ weight and body fat were held to monitor their progress and foster compliance.
Promising results were recorded following the 12-week intervention. Researchers saw significant reductions in energy and fat intakes, while intakes of protein and fibre increased. Participants were also eating slower (taking longer than 20 minutes for their meals), while the proportion of late-night eaters and those who skipped breakfast decreased.
PERSUADE also encouraged participants to obtain their nutrients from real foods as opposed to supplements, and the data showed supplement consumption dropped from 29.2 per cent to 4.2 per cent at post-intervention.
Researchers also reported a significant increase in the number of physically active peers after three months, while the proportion of smokers declined from 16.7 per cent to 4.2 per cent.
A blueprint for reversing metabolic syndrome?
Researchers note that the success of peer support appears to be due in part to the non-hierarchical, reciprocal relationship that is created through the sharing of similar life experiences.
But Dr Amutha says peer support in healthcare has been used effectively to combat obesity, diabetes, hypertension and cancer. The current study adds to the growing body of evidence supporting group-based peer support lifestyle interventions to improve metabolic syndrome-related risk factors in adults.
Read more: Type 2 diabetes: is it what you eat, or how much?
"Since peer support promotes activation of public members to have the same health goals by promoting collective behavioural changes, the framework is seen to substantiate lifestyle intervention better than a standalone lifestyle intervention," she says.
She adds that consistent and continuous support of peers is essential to ensure significant changes in lifestyle behaviours within a shorter period of intervention (less than 12 weeks).
"PERSUADE encouraged the peers to share experiences, and learn more about the barriers faced by peers to practise healthy eating and regular physical activity during the 12-week intervention period,” she says.