
If there was a health condition that affected around one in seven men, that severely reduced their enjoyment of life, put them at significant risk of developing depression and/or anxiety, and was the biggest reason why they may not become fathers – do you think we would have heard of this? And would you assume that doctors would know about it, know how to look for it, and how to treat it?
It seems almost inconceivable that we wouldn’t have a massive public health awareness campaign, a school education program, celebrity ambassadors (a famous cricketer or two) and perhaps even the prime minister urging men to get checked out.
Such a condition does in fact exist, but in women not men. And there are no public health campaigns or celebrities raising it as an issue, and most of us have never heard of it. Not even the estimated 70 per cent of women who have it, know about it.
Why?
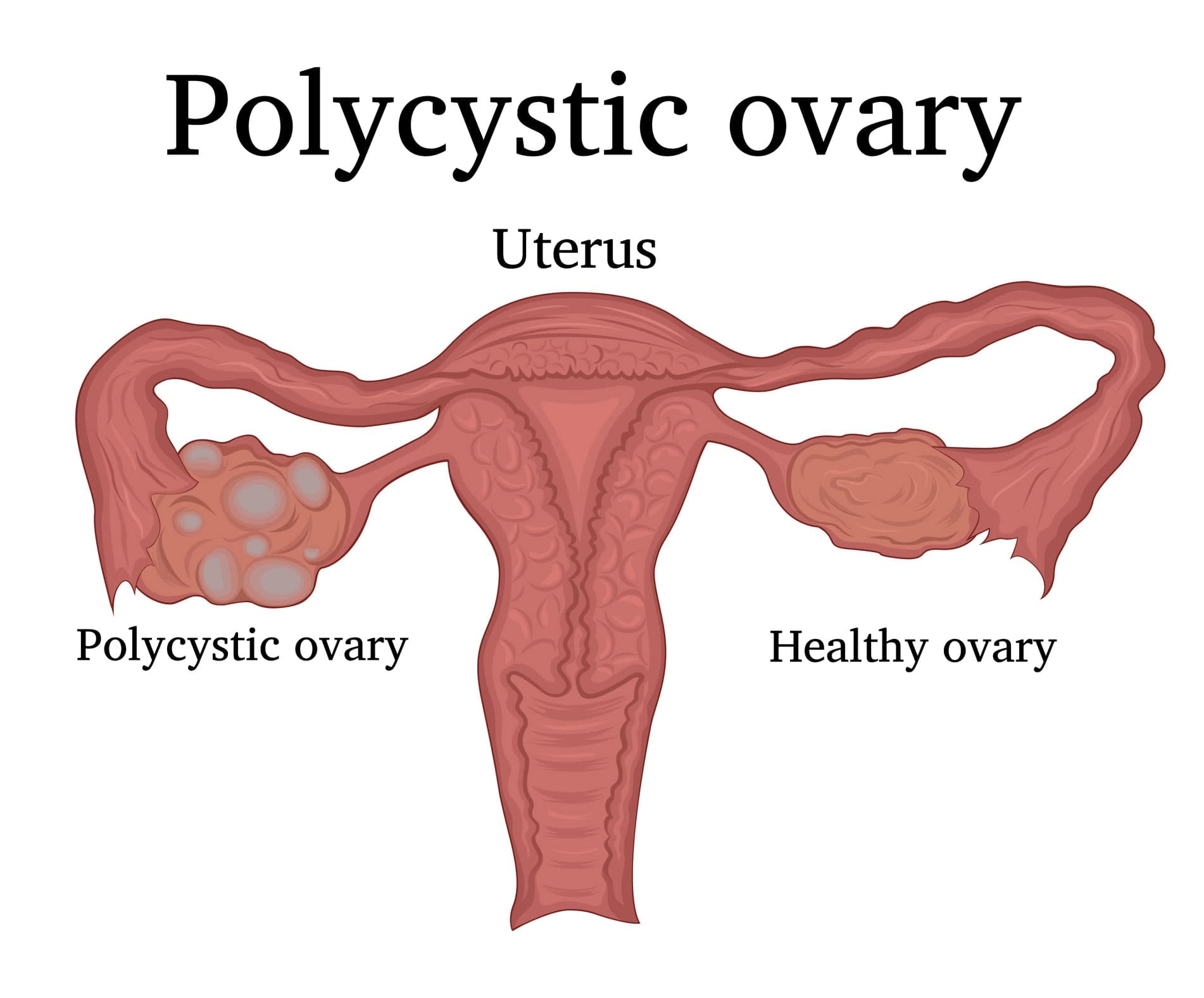
Polycystic ovary syndrome (PCOS) is the most common hormone condition affecting women in their child-bearing years. It increases the risk of metabolic conditions (diabetes, diabetes in pregnancy), reproductive issues (infertility and endometrial cancer) and psychological conditions (anxiety, depression and mental health disorders).
Listen to experts talk about PCOS
PCOS is the main reason why women have trouble getting pregnant, and it causes symptoms that can be very difficult to deal with such as acne and body hair in highly visible places such as the face. Affected women also have a high risk of depression and anxiety, and to top all that off, weight gain and obesity are common. Between 8 to 13 per cent of women have PCOS, and in Indigenous women it's up to 21 per cent.
And if all of this was not enough, women find it hard to get a clear diagnosis, good management and high-quality information. In fact, some women are told by doctors, or read inaccurately on the web, that they are likely to be childless for the rest of their lives, causing extreme distress.
So, how could this highly unsatisfactory situation be improved?
Professor Helena Teede, a treating endocrinologist, became overwhelmed by the scale of the problem before deciding to partner with women and other health professionals to fix it.
Firstly, she talked extensively to women with PCOS on what was important to them (radical even today). But it was what she attempted next that would have quelled the enthusiasm of most mere mortals.
She consulted the leading global PCOS experts and convinced them to set aside the usual barriers to collaboration and create a robust, definitive body of work that would be adopted worldwide.
That all 38 societies and experts agreed to work over a three-year period, across six continents and 71 countries to create the first International Evidence-Based Guideline for the Assessment and Management of PCOS, is a testament to Helena’s endurance and tenacity.
Now Monash University in Australia is leading the world in PCOS research, but more importantly driving health impact.
On average it takes about 17 years from ‘bench to bed’ before research findings are implemented. At which time of course, the research has been superseded. Guidelines aim to drive evidence into practice quickly, yet no matter how extraordinary in terms of depth and scope, a guideline doesn’t impact lives unless or until it is adopted.
That is where I came in.
As a research translation expert, my role was to find innovative ways to get the attention, and support, of practitioners, who are inundated with evidence, to adopt the guideline. And, to raise the health literacy of women with PCOS.
This is what we did
Firstly, we co-designed a range of clinical practice decision tools including algorithms and ensured a high level of palatability among GPs, who are the central care coordinators.
Secondly, we harnessed the influence of the global experts to disseminate the guideline within their networks and across 81 of the most esteemed international conferences in 2018/19.
Thirdly, we simultaneously published in three high-impact journals, across the three disciplines of endocrinology, fertility and reproduction. And supported this with published translation tools, including our app (see below). To our knowledge this breadth and scale has not been done before.
In tandem, we focused on the most important aspect of this work; that is how to support affected women.
By developing a ground-breaking partnership with the Monash Faculty of IT we co-designed and launched the first evidence-based PCOS app (AskPCOS), available on Apple and Google.
Women across 100 countries are now using the app that has just been shortlisted by an international body as one of the world’s top 10 apps most likely to change the lives of girls and women.
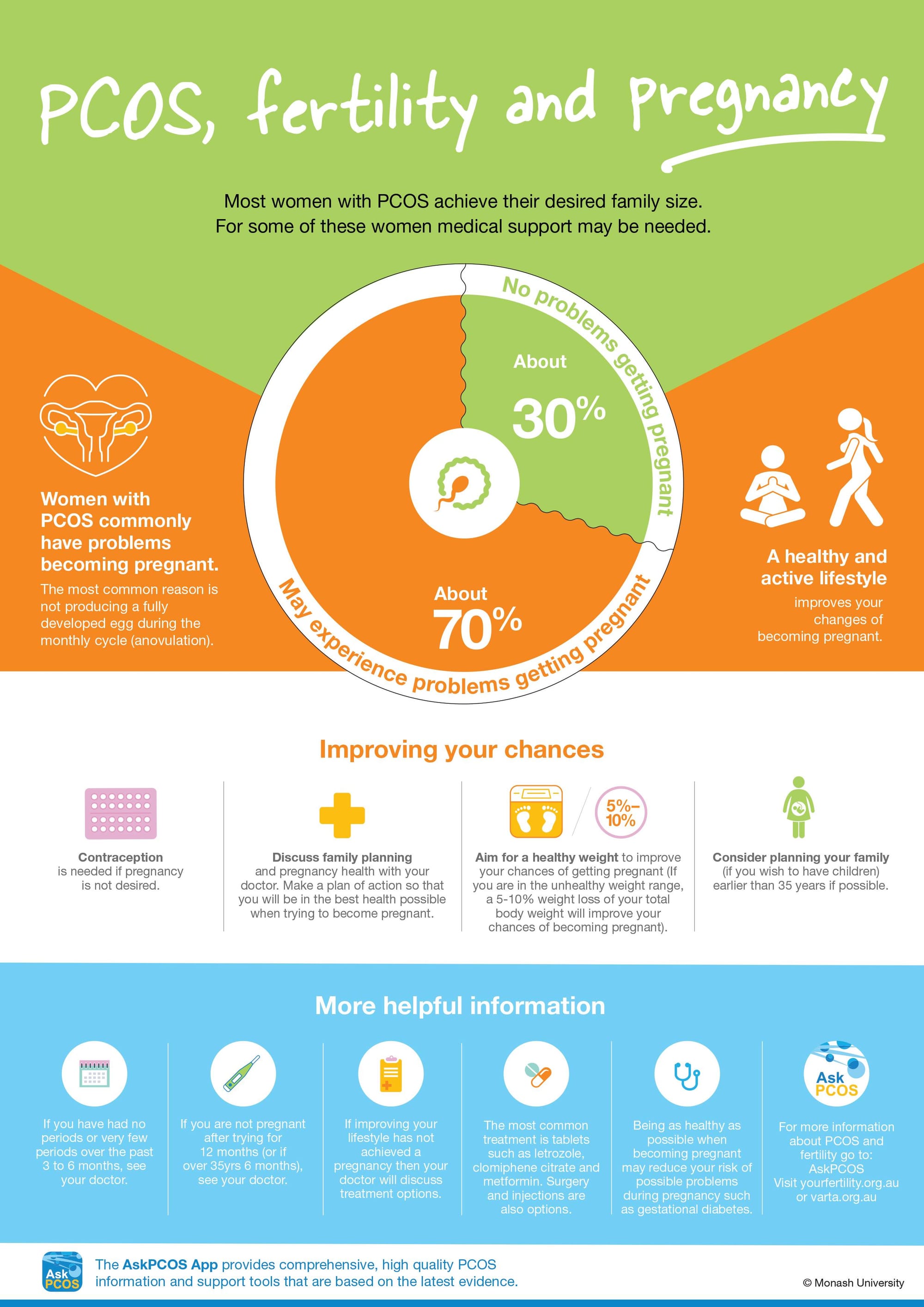
We are incredibly proud of the reach of this work, to reduce access inequalities to high-quality health information to girls and women. We also created a range of other co-designed resources.
This includes a highly engaging learning module for health practitioners. It is evidence-based and draws inquiring practitioners together from around the world to learn, discuss and ultimately become change agents in delivering best-practice PCOS care.
The module builds knowledge, and presents engaging real-world case studies to assist in the implementation of an evidence-based approach to the assessment and management of PCOS.
Uniquely, the global platform asks participants to consider controversial aspects of care and encourages discussion with practitioners from all over the world.
The culmination of this work has been an extraordinary global reach within the medical profession and among girls and women.
Learn how to better diagnose and manage polycystic ovary syndrome (PCOS) through the online course, Polycystic Ovary Syndrome: An Evidence-based Approach, accredited by RACGP and ACRRM.





