Humans have been aware of their heart rate for thousands of years. But knowing the meaning behind the beats isn’t so simple.
Myriad factors affect our heart rate, including our age, medical conditions, medications, diet, and fitness level. Today, we’re even more aware of our heart rate, thanks to devices such as smartwatches that can measure every beat during rest and exercise. So, what is normal?
How should we measure our heart rate?
Surprisingly, there are more than 12 places you can feel your pulse. But there are two that are the easiest and most reliable – the radial artery, which runs along the inside of the forearm from the base of the thumb; and the carotid artery, which runs up the front of the neck two fingers to the side of the Adam’s apple.
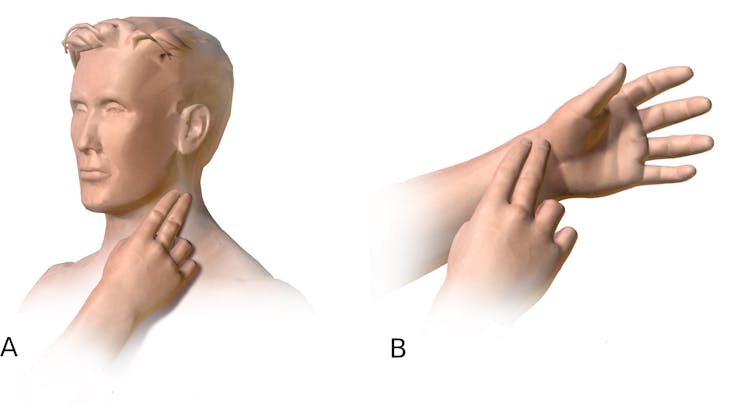
The best way to measure heart rate is to sit down for a few minutes and relax, then use two fingers (not your thumb, as its own pulse can confuse your measurement) to gently compress the artery and count the beats over 15 seconds. Multiplying this by four will give your heart rate in beats per minute.
If you’re using the carotid, it’s important to only check one side at a time, and not to massage the artery – this is an area that senses blood pressure flowing through the artery and signals to the heart to keep it in a tight range; stimulating this area can trick it into dropping the heart rate and blood pressure, leading to a blackout.
Your heart runs on electricity – in fact, every single heartbeat is the result of a tiny electrical impulse travelling through your heart muscle. These impulses can be measured using an an electrocardiogram (ECG), which is the most reliable and informative measure of your heart rate. The test is non-invasive, painless, and you can get it at most GP practices and pathology services.

Wearable devices such as smartwatches use light, rather than pressure, to measure heart rate. As the volume of small arteries in the wrist transiently increase with each heart beat, the amount of light reflected back to a conductor in the watch changes – and the frequency with which these fluctuations occur is the heart rate.
They’re an attractive way to have real-time heart rate recording during rest and activity, but they have inherent limitations due to the simplicity of their design, and interference caused by movement can often interrupt their recordings.
Read more: Gut health: Investigating the role a high-fibre diet can play in controlling high blood pressure
What is a normal heart rate and what affects it?
As an adult, the normal range for resting heart rate is 60 to 100 beats per minute. This applies for anyone over the age of 17 – infants and children have faster heart rates due to their smaller body and heart size. This “normal” range for heart rate doesn’t change across the adult lifespan.
Lots of things can cause your heart rate to speed up (known as tachycardia):
- Exercise. When you exercise, your heart rate needs to increase to pump more blood around your body. A normal person pumps about five to six litres per minute, and an average person can get up to 20 litres a minute while exercising – athletes can even go as high as 35.
- Coffee and energy drinks. Caffeine increases your heart rate by blocking adenosine. This a chemical in the brain that causes drowsiness and slows heart rate.
- Stress. Stress and excitement cause activation of the sympathetic nervous system, which was biologically designed to help us hunt for food or run away from animals. But in the modern day it tends to be activated more when we have a difficult conversation at work, or watch Game of Thrones.
- Infection. Serious infections, particularly when they spread into the bloodstream (sepsis), put more strain on the heart as more blood flow is required to carry immune cells from the bone marrow and lymph glands to target the infection. A faster heart rate alerts doctors the infection is severe.
- Thyroid disease. Your thyroid is a gland in your neck that works to maintain your metabolism – an overactive thyroid gland can increase the heart rate, along with causing weight loss, irritability, heat intolerance and diarrhoea.
- Heart arrhythmias. The heart’s normal electrical activity can also be interrupted, leading to tachyarrhythmias, where the heart is beating fast and abnormally. Atrial fibrillation is the most common arrhythmia, where the pulse becomes irregular, and can cause symptoms such as palpitations, shortness of breath and light-headedness. One of its more serious complications is stroke.
Read more: Getting to the heart of the matter on stroke
What about going slow, or bradycardia? Again, there are a few common reasons:
- Relaxation. The heart rate slows as we relax, and the counterpart to the sympathetic nervous system, the parasympathetic nervous system, which helps us to “rest and digest”, is activated.
- Medications. Many tablets can slow down heart rate (some deliberately to ease the load on the heart), such as beta-blockers, antidepressants and opioid-type painkillers.
- Physical fitness. Exercise training and cardiovascular fitness causes a lower resting heart rate, and it can be quite normal for athletes to have resting heart rate in the 40s. It’s not entirely clear why this happens, but the predominant mechanism behind it is changes to the electrical conducting system of the heart that happen with exercise training.
- Heart arrhythmia. Arrhythmias can also slow down your heart. Heart block occurs when the electrical signals, which originate at the top of the heart in the atria, aren't conducted properly to the ventricles at the bottom of the heart. This can be life-threatening, as although the ventricles have an intrinsic backup system to beat at approximately 40 beats per minute, this can fail and cause the heart to stop completely. There are various types of heart block, which range in severity from no symptoms at all to frequent blackouts or sudden death. Those at the more severe end of the spectrum may need a pacemaker to stimulate the heart to beat.

What heart rate should we aim for?
Although the “normal” range of heart rate is quite broad at 60-100, there’s increasing evidence that having a heart rate at the lower end of the spectrum is better for you.
In a large US study, a higher heart rate was associated with a greater incidence of heart attacks, strokes, heart failure and early death from heart-related and non-heart-related causes. In patients who have a history of heart attacks, having a lower heart rate seems to be better, and we often give tablets to slow down the heart.
But the converse is true when we exercise. Most people’s peak heart rate when exercising should be no more than 220 minus their age (so, 190 for a 30 year old, 160 for a 60 year old). If your heart rate is more than 10-20 beats higher than your age maximum when exercising, this could be due to abnormal conduction of the heart.
“Chronotropic incompetence” is when the heart is unable to increase its rate in proportion to increased demand (exercise), and it’s a bad sign when the heart can’t lift its rate as much as it needs to. The ability of the heart rate to drop back down to normal after exercise is also important (heart rate recovery) – failure to do so also predicts a higher probability of early death.
Can I change my heart rate?
More important than trying to reach a lower heart rate is just trying to do more of the things we know keep us healthy. Plenty of exercise (at least 30 minutes five times a week at moderate intensity), relaxation, a healthy diet, and keeping a careful eye on your blood pressure and waistline will all help.
Wearable devices are great at providing you with heart rates, but be aware they’re not always accurate, and if you’re getting abnormal readings, particularly if you have symptoms, then you should see your doctor.
Shane Nanayakkara receives funding from the National Heart Foundation and the Baker Heart and Diabetes Institute.
Anna Beale does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
This article originally appeared on The Conversation.