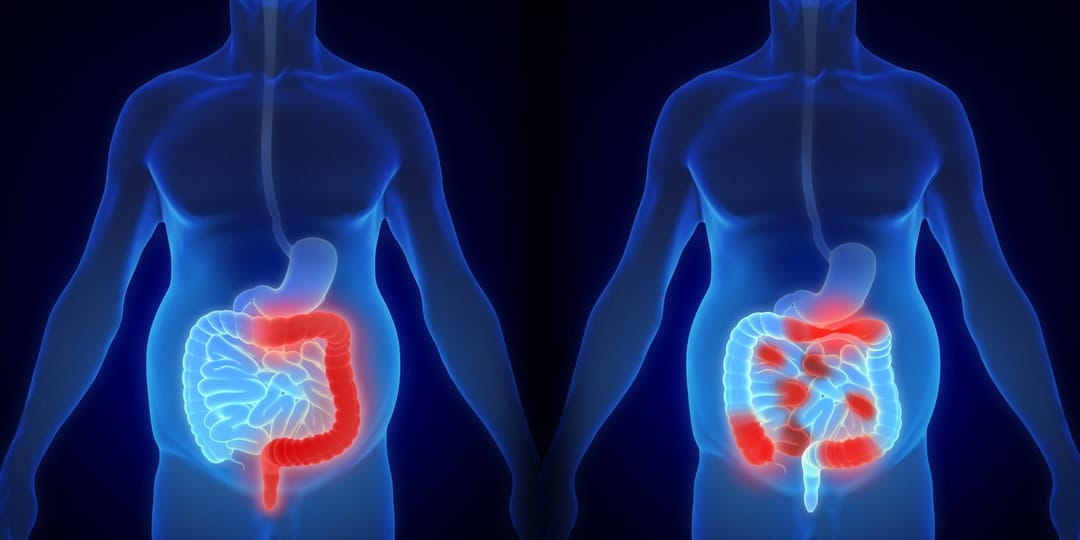
Inflammatory bowel disease (IBD) is not one single thing. It's a lifelong autoimmune inflammatory condition of the gastrointestinal tract that can lead to hospitalisations, surgery, and a decreased quality of life.
The two most common forms of IBD are Crohn’s disease and ulcerative colitis. The causes of IBD appear to be a blend of environmental and genetic factors. So, in brief, it's called a "complex disorder". Almost 75,000 Australian suffer from IBD, one of the highest rates in the world.
The most effective treatment for controlling the immune system response are "biologics". Biologic therapies, which include complex antibodies that block important communication between the immune system and the inflamed intestine, have revolutionised the modern management of IBD.
Optimising their use is important. On one hand, they're expensive and suppress the immune system, but, on the other, they can be highly effective. However, about one-third of patients can lose response to whichever drug they're taking and need further tailoring of their therapy.
Dr Mark Ward is a gastroenterologist at Alfred Health, and a Monash University researcher. He's been working with IBD patients for years. Following a fellowship at St Thomas’ Hospital in London, he took the lessons he learned about virtual clinics back to Alfred Health.
He's also the senior author on a recent study published in Alimentary Pharmacology and Therapeutics that outlines the remarkable improvement in both patient outcomes and quality use of therapy using a virtual clinic, compared to standard outpatient care, for the most challenging cases of IBD.
What is a virtual clinic?
A virtual clinic consists of bringing together a multidisciplinary team of the relevant medical practitioners, including a gastroenterologist, pharmacist, and IBD-nurse specialist to coordinate delivery of compassionate intensified treatment to patients who are sick and losing response to therapy.
They review the patient’s progress from the electronic patient record, along with results of investigations, to make informed decisions about the patient’s treatment, and then review outcomes on a six-monthly basis. The group’s early experience was extremely positive.
“With our colleagues at the Austin Hospital and Eastern Health, we set up a study to compare the virtual clinic model to the standard outpatient care, in patients losing response to anti-TNF therapy,” Dr Ward said.
“What we found with the virtual clinic was a remarkable improvement in both patient outcomes and quality use of therapy.
“The rate of successful treatment de-escalation was also doubled, which is important – we don’t want to over-immune-suppress our patients, and these therapies are expensive.”
The study incorporated 149 patients, with 69 treated using the virtual clinic model, and 80 patients with the standard outpatient care.
Effective treatment success was seen in nearly two-thirds of the virtual clinic patients, compared to a third in the outpatient group, with twice as many patients undergoing appropriate dose intensification. Rates of tight (objective) disease monitoring were nearly tripled.
Dr Ward said: “In a typical outpatient clinic, one has very limited time to assess and manage a complicated sick IBD patient.
“More tests are often needed, which requires further appointments, and a delay in delivering effective treatment. The virtual clinic helps get around this; we can make decisions, supported by the results of non-invasive tests and therapeutic drug monitoring.
“This facilitates a ‘treat-to-target approach’ – healing the bowel, rather than relying on symptoms alone.”
'What we found with the virtual clinic was a remarkable improvement in both patient outcomes and quality use of therapy.'
He said that 30 to 50 per cent of these patients will need biologic therapy.
“Treating these patients is not straightforward,” he said. “Are their symptoms due to active disease? Where and how severe is the disease? What tests and interventions are needed? Which is the best biologic? What dosage of medication is needed? Are they responding well? Can we optimise their treatment?
“We’ve had greater capacity to personalise the patients’ care, and to be consistent in our approach.”
The Alfred group pioneered this approach in Australia, and there's now increasing uptake of virtual clinics in IBD centres around Victoria, and Australia.
“We’ve found that a collegiate, collaborative approach has really fostered relationships, data sharing and, hopefully, use of the protocols in other hospitals around Australia,” Dr Ward said.
”Given the current COVID-19 pandemic requirements for physical distancing, we need new models of care which not only manage patients for a better personal outcome, but also virtually or remotely to avoid them coming into hospitals.”
This study was supported by a GESA Ferring IBD Clinical Project Award (Gastroenterology Society of Australia)





