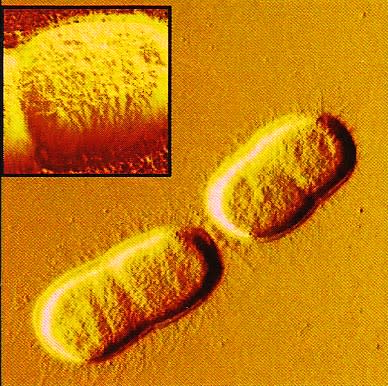
The superbug Acinetobacter baumannii (AB) is high on the most wanted list of global superbugs - infections that current antibiotics can’t kill or have trouble killing. It is resistant to most of them, even a last-line (or last resort) uber-antibiotic called colistin.
According to Monash University’s Associate Professor John Boyce, a molecular biologist, this is what AB is like: “A very nasty bug, but not something in general that people in community are going to get. It goes for people who are already very sick, especially patients in intensive care units. It is very good at living on surfaces and very difficult to kill.
Watch the latest episode of A Different Lens: Beating the Superbugs
“What tends to happen is that the AB bacteria live on surfaces, on taps, sinks, hospital devices and it’s very hard to eradicate – then patients who are very sick, and may have in-dwelling devices like ventilators develop an AB infection. This then quickly leads to pneumonia or bloodstream infections, and the mortality rate of patients in ICU’s with these infection is very high, up 30 to 50 per cent.
“In the past we have had antibiotics that we could use to clear these infections,” he says.
“Even fifteen years ago there was not much problem with AB. It could be treated and cleared. Now that’s not the case. Most strains are multi-drug resistant.”
In other words, like the other five worst superbugs on the global ‘ESKAPE’ list* (ESKAPE’ is an acronym using the names of the bugs), it is a monster, constantly evolving and mutating and so far more durable than anything we can throw at it.
Associate Professor Boyce is part of an international team about to begin a new five-year investigation into the superbug, its resistance mechanisms and also novel (new) treatments for infection. The National Institute of Health in the United States have awarded the team $US3.4m – team members are from the University of Florida, Case Western Reserve University in Cleveland and Monash.
Leading the project is Associate Professor Jürgen Bulitta of the University of Florida’s department of pharmaceutics; there is a strong pharmacology aspect to the research. Associate Professor Bulitta spent four years at Monash’s faculty of Pharmacy and Pharmaceutical Sciences in Melbourne, until 2015. During that time the pair often worked together, and the partnership continues.
“We do the molecular biology part here at Monash” Associate Professor Boyce says. “We do genomic sequencing to see how the bacteria changes in response to different antibiotics, and we analyse the transcriptome, which is a reading of the genes that get expressed, and what changes occur in the presence of the antibiotic and ultimately lead to resistance.
“Pharmacy’s role, which Jürgen leads, is trying to come up with the best antibiotic combinations for use in clinical settings. They are not trying to develop new antibiotics – they are trying to combine the ones that are already available in ways that are more useful than they are now.”
Recently Associate Professor Boyce was part of a team (which included Portuguese researchers) that discovered the reason that AB from a bloodstream infection could not be cleared from an elderly Portuguese patient even after colistin treatment, the seventh antibiotic the patient had been given in hospital. The strain developed “high-level” colistin resistance during treatment due to a very specific mutation.
If you can kill the whole population quickly, which is how antibiotics are supposed to work, resistance won’t arise.
He agrees that trying to combat these powerful infections – for molecular biologists, pharmaceutical scientists and all health researchers involved in the quest – is endless, a constant game of catch-up. But they have to do it otherwise more people will die needlessly.
“The reality is that for all of the current antibodies that are available you will find resistance mechanisms will evolve over time. There’s no way around that. It’s really a race to keep ahead of the game. In the past we have kept ahead of the game with new antibiotics with new targets. The bacteria haven’t seen them before and it might be five to ten years for resistance to develop. But it will happen in the end.”
Read more Sleepwalking towards an antibiotic apocalypse
Associate Professor Boyce says two factors conspire to complicate the race to beat the superbugs. The first is antibiotics being used incorrectly in clinical settings, and the other is the lack of new, more powerful antibiotics on the market.
“So we have to come up with new ways to do things,” he says. “Our priority with this project is about trying to extend the lifespan of current drugs we have to try and keep them usable in some way so that we can wait until new drugs come onto the market over the next five – ten years but not be in a situation we have nothing until then. It’s taking what we have available to us right now and repurposing that so it is effective.”
He says if antibiotics are poorly dosed in hospital settings it can be counter-productive. “Resistance comes more easily when antibiotics are used incorrectly, ineffectively and inefficiently. You let part of the bacterial population survive a treatment and the longer they grow in the presence of that antibiotic the more likely they are to build up resistance mutations. If you can kill the whole population quickly, which is how antibiotics are supposed to work, resistance won’t arise.
But if the dosages in a patient are not enough to kill the bacterial population the bacteria have a better opportunity to grow and mutate.”
*ESKAPE list
- Enterococcus faecium.
- Staphylococcus aureus.
- Klebsiella pneumoniae.
- Acinetobacter baumannii.
- Pseudomonas aeruginosa.
- Enterobacter.
Find out more about this topic and study opportunities at the Graduate Study Expo





