If you have males in your household, wee on the floor is probably no surprise to you. This may not be a big problem in a small household, but if you have hundreds of urinals, that adds up lots of urine on floors, causing slipping accidents, and fetid smells.
So, how do you get men to pee straight? Give them a nudge.
Schiphol Airport in Amsterdam solved its floor urine problems by painting a house-fly on the ideal pee spot in the urinal. It worked – 80% reduction, and few had any idea they were being schooled in peeing in the zone.
So, whether you create piano stairs, house-fly urinals, or reduce the size of dinner plates, you’re exploiting the subtle art and science of influencing behaviours. This may sound sinister, but as the author of The Nudge, Richard Thaler, points out, we’re doing this all the time:
“The first misconception is that it is possible to avoid influencing people's behaviours and choices.”
Influencing people to optimise health has never been more important than right now. Pandemic choices are life, illness, and death decisions. But more than that, they’re choices we all make on behalf of those we love, and they can have extreme consequences for the vulnerable in our communities.
Read more COVID-19: Is getting vaccinated really part of the social contract?
It’s hard to recall a time in recent history when the aggregation of our individual behaviours and choices so directly equates to who will live, who will live free of illness, and who will die.
So, how do we partner with people to enable them to make evidence-based, health and life-protecting choices in a pandemic?
Behavioural science has some answers
Our national study, based on behaviour change models, has shown that most Australians reported adhering well to public health measures during the second COVID wave (May and July 2020).
Three-quarters of us stuck to the rules, while one-quarter felt less compelled to physically distance, self-quarantine if unwell/diagnosed, and to not get tested at the onset of symptoms. Young men in cities reported lower levels of concern or motivation to comply.
Perhaps surprisingly, there was strong support for government lockdown measures, which the majority (81%) considered important and appropriate (75%).
So, what does this study tell us about a formula to enhance public compliance with health measures in a pandemic?
Singing from the same song sheet was critical. Successful second-wave suppression required consistent communication from political and health leaders.
We saw the importance of this “writ large” in the UK when Prime Minister Boris Johnson introduced the “Stay alert, control the virus, save lives” campaign.
Critics labelled it confusing and nonsensical. It even incited rebellion in some, with the Scottish First Minister Nicola Sturgeon countering that “Stay home” would continue to be her message to Scotland.
Conversely, Victoria was a very good example of providing a unified and consistent approach. News conferences were co-led by the Premier and the CHO, who both provided supportive and simple public health messaging.
Also, it’s critical that adequate economic strategies are provided to prevent people having to break the rules to survive. Victoria provided a range of funding support for testing, isolating, and to stay afloat due to lost income.
The very good news
At the time of writing, elected officials are locked inside the Victorian Parliament enduring a marathon battle to pass the pandemic bill, while outside protests continue, complete with wizards and hanging gallows, and the new variant Omicron ominously slips past border controls.
But there is good news.

The very good news is that vaccines are clearly working. Hospital rates in Victoria continue to trend down (currently below 300), and as we move closer to claiming our trophy as one of the most vaccinated regions in the world (93% first dose, 90.1% second dose), we’re also looking good for booster acceptability, too.
Our data shows 77% of people are likely to get a booster (August 2021). The rates are much higher in older groups (88% for those aged 65-plus), with acceptability diminishing a little down the age gradient (75% in those 35-64: 73% in 18-34).
What’s behind Victoria’s high rate of vaccine uptake?
Knowledge, beliefs and attitudes of individuals are the factors that direct behaviours. Our research shows that the Victorian government has had a high level of trust and social licence, which has enabled the public to adhere to public health measures.
Clear and consistent messaging on what matters most to Victorians – protecting others, knowing that the vaccine is safe and effective, getting a doctor’s recommendation to get vaccinated, balancing opening up with ongoing public health measures where needed – will continue to be vital.
And we need to work harder to understand the differences that drive those who are as yet unvaccinated, and what strategies, based on behavioural science, may help encourage vaccination is important (see graphic).
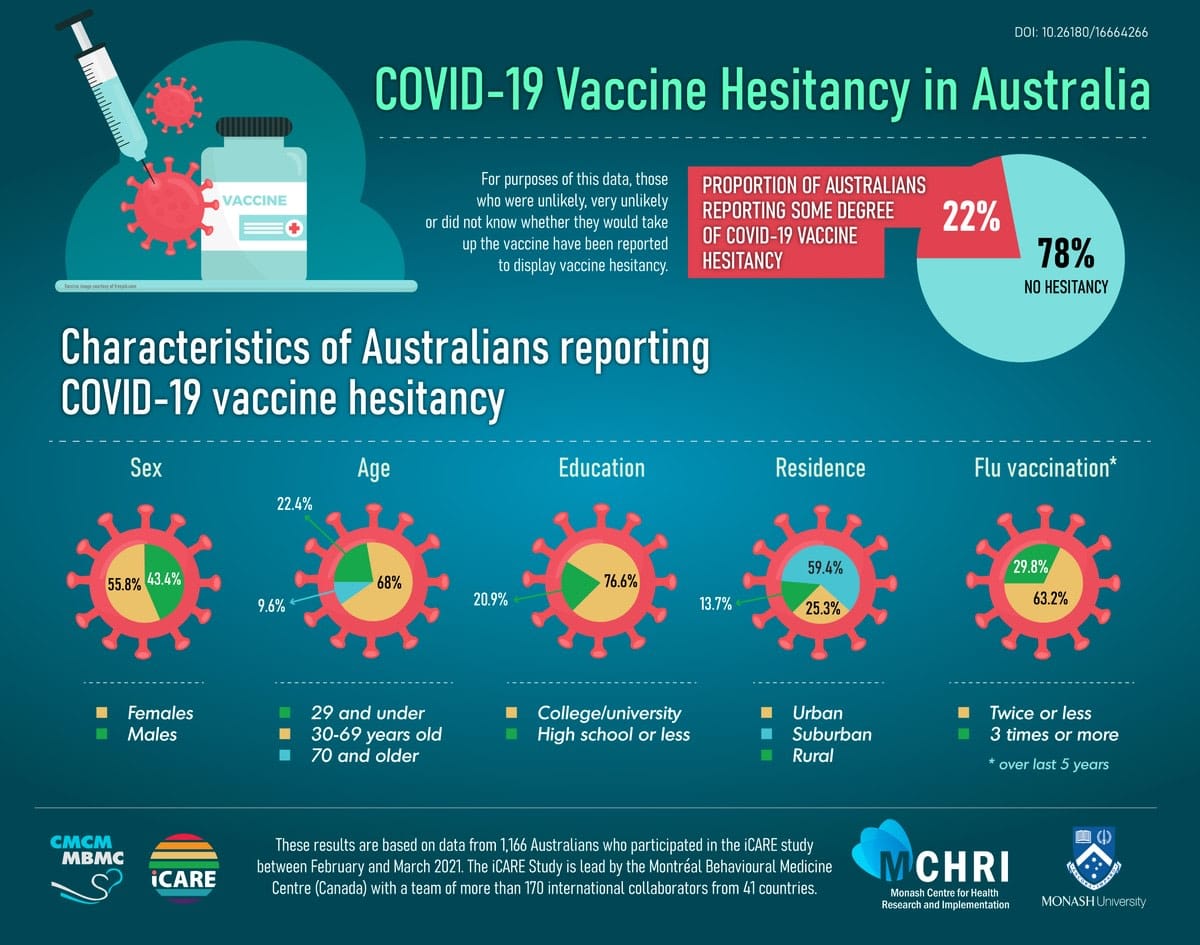
Managing misinformation, and highlighting safety and efficacy of the vaccines appear the most influential strategies, while mandates, and even freedoms for the vaccinated, appear less likely to be successful without addressing the safety and efficacy concerns that are most important to those still unvaccinated.





