
The Monash University FODMAP app is celebrating its fifth birthday this week.
Not familiar with this acronym? Count your blessings. Maybe you’re one of the lucky ones. You don’t have bloating and excruciating gas pains after eating. You don’t have to scout toilet facilities everywhere you go in case you have an attack of diarrhoea. You are not on a first-name basis with a dietitian. You may never even have consulted a gastroenterologist! In short, you’re probably not one of the one in seven people who suffer from irritable bowel syndrome (IBS).
For the rest of us, the Monash University FODMAP app can be a life-changer.

First, a little background. In 2005, Monash’s Department of Gastroenterology launched a major study to see if IBS could be managed through diet. The research team found four classes of short-chain carbohydrates that were poorly absorbed in the small intestine. These sugars attract water into the bowel, and when they reach the large intestine, they’re fermented by the resident gut bacteria. This, in combination with a sensitive gut, is what results in IBS symptoms – bloating, distension, pain, constipation and/or diarrhoea.
The researchers gave these culprits the name FODMAPs, which stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. The team, led by gastroenterologist Professor Peter Gibson and nutrition scientist and dietitian Associate Professor Jane Muir, found that patients were successful in reducing or even eliminating their IBS symptoms by eating less of the specific FODMAP-containing foods that bothered them.
As the team tested foods for their FODMAP content, they published the results in a paperback booklet for dietitians to share with patients. This valuable resource gave dietitians a blueprint for identifying patients’ individual sensitivities and tailoring a personalised diet around them. But because new foods were constantly being added, the booklet was out of date almost as soon as it was published. “Patients would call me from the supermarket,” recalls Muir, “asking if this or that food was on the list.” And what about patients without access to a dietitian?
With just a $20,000 grant, Muir hired a Monash IT graduate to build a smartphone app. Five years ago, on December 17, 2012, the Monash University FODMAP app was released. It promptly rose to the top of the charts.
“It has been the No.1 paid medical app in Australia ever since it was released,” says Muir. It’s in the top 10 paid apps overall in Australia. It has been downloaded in more than 120 countries and is among the top medical apps in many of them."
The success stories from patients started rolling in.
“You've changed my life! With your app I have been able to learn which foods are OK to eat and which aren't ... my quality of life has increased dramatically over the last couple months. THANK YOU!"
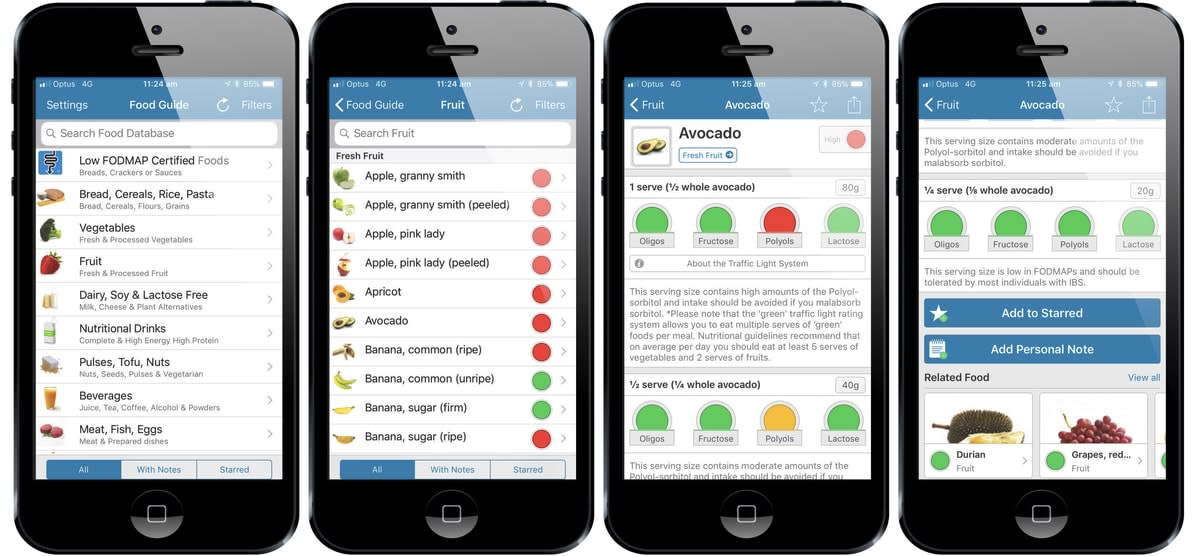
For $12.99, users get continuing access to the team’s database of the FODMAP content of various foods, which is displayed using a multi-level traffic light system. The app also includes extensive background information about FODMAPs, a symptom diary, a shopping list, recipes and feedback channels to the FODMAP team. There are no in-app purchases. All the money earned from the app goes directly back into research and testing at Monash.
The price – high for an app – is deliberate, says Muir. “It’s a therapy. it's like going to a chemist to buy a therapeutic product (such as a probiotic). You don't expect to pay $10 for a probiotic. You pay more. It's a therapeutic treatment for your condition.”
The app is designed to be used with the guidance of a dietitian, says Muir. Once a positive diagnosis of IBS is made (and coeliac disease, inflammatory bowel disease and colon cancer have been ruled out), he or she can use the app to figure out how much of the various FODMAPs will trigger symptoms, and stay below that threshold. This is important because many high FODMAP foods are nutritious and should be part of a healthy diet. “We don’t want people over-restricting. Some of these foods are prebiotics that feed healthy gut bacteria,” says Muir.
For example, on the top level, an avocado might be a “red light” food. When the user clicks through, they find a typical serving size – half an avocado – is high in polyols. When they change the serving size to a quarter of an avocado, the light turns yellow; at an eighth – the amount you might add to a sandwich – it’s green. No need to avoid avocados, then, even if you’re sensitive to polyols. Just be careful not to eat too much at once. “It’s not a no FODMAP diet; it’s a low FODMAP diet,” says Lyndal McNamara, a dietitian with the Monash FODMAP team.
“We get a lot of feedback on the app – new features that people would like to see and what we could do to improve it,” says McNamara, who is part of the team that manages the popular Monash FODMAP Facebook page (44,000 followers) and Twitter feed (10,000 followers). “We use that to inform future updates and development. At the end of the day we do want it to be the most useful tool that it possibly can be.”
The app’s spectacular success was a bit of a surprise to the researchers. Muir and her team have had to navigate a steep learning curve. “I just thought it would be a little thing, a handy guide, to help fund some research,” says Muir. “I had no idea it was going to turn into the business that it has, with one thing leading to another thing to another.
“As a scientist, I didn’t ever think I’d ever be in this sort of commercial business world. I do appreciate now that we should be translating our research out into the community. It’s no good having all this wonderful knowledge and people don’t know about it. But to translate your research out, so that everyone knows there’s this wonderful diet to help this medically diagnosed condition, is extremely expensive and difficult to do.”
Success is a good thing – but it creates its own set of challenges. Copycat apps. Websites and cookbooks that lift copyrighted Monash FODMAP material. “Everyone’s competing and copying us, and they don’t do it very well,” says Muir. “The information is often wrong or incomplete. They’ve got a different agenda – they just want to make money.”
The Monash team has worked to stem this tide by making an intensified effort over the past year to cement its place as the undisputed FODMAP research authority. There’s a new website, monashfodmap.com, and a new logo and trademark. The FODMAP Grand Tour Down Under video (328,000 views on YouTube), has been relaunched with the new branding. The app is being translated into other languages, with French and Spanish versions currently in the works.
They’re supporting innovation in food industry by offering certification for food manufacturers. “Companies are popping up everywhere to address the need for low FODMAP products, and existing companies are expanding their range or reformulating their products to make them more suitable,” says McNamara. Products that have been tested and certified by the Monash labs can carry the Monash University FODMAP logo and trademark on packaging. They’re also promoted on the Monash FODMAP Facebook and Twitter platforms. In Australia, Carman’s, Arnott’s, Brumby’s Bakery, Massel and S(o)me Foods all have Monash Low FODMAP Certified™ food products. Other companies around the world are following suit, including Nestle Health Science, FODY Food Co and Schär.

To address the gap in trained dietitians and health professionals, the team has developed a self-paced online training program for health professionals. Once they’ve successfully completed the 10-module course, dietitians and nutritionists all over the world can advertise their Monash University FODMAP training, giving gastroenterologists and GPs good options for referring patients.
Millions of people’s lives will be changed for the better thanks to this little blue logo. “The money comes back to fund research, the app and education; it’s not something that’s going into anybody’s back pocket. It all comes back to the University, which is for the common good. It’s ticking all the boxes of what Monash should be about,” says Muir.
“I cannot tell you how much my life has changed for the better since downloading the app and taking on some of the guidelines. Also watching the video on your website was such an incredible moment. I felt like someone finally understood how I’ve been feeling for so long. Hallelujah! I am a 42-year-old female who has lived with pain and discomfort since I can remember. I have only used the app as a general guide but the change seemed to happen overnight. I no longer sit at work in pain with the bloating and cramping, and can wear normal clothes again as my stomach is not so blown-out and sensitive. I can’t thank you enough. The work you are doing is changing people’s lives."





