Imagine it's 2030. Ten-year-old Amy is wheeled into a children’s hospital clinic by her mother and, across town, 45-year-old Anh is visiting his oncologist one week after leaving hospital for his lung cancer operation.
Amy is slowly losing her ability to walk due to a muscle disorder that has only recently been given a name. Many diseases of muscle in children such as muscular dystrophy are caused by gene mutations (muscle disorders in adults are less likely to have a genetic mutation basis). In 2018, only about 40 per cent of these mutations were known.
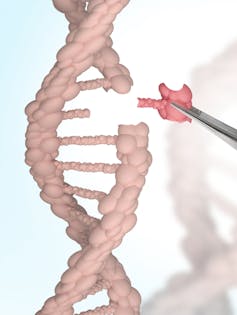
In 2030, we know 99 per cent of mutations causing inherited muscle diseases worldwide. Because the costs of genetic sequencing are so much lower, more people have had their genomes scanned. Researchers have spent the past 20 years gathering information about various genetic markers and mutations into massive biobanks. This data is now globally accessible, which has led to international collaboration and better understanding of diseases.
So, 2030 is seeing a boom in precision medicine – where some diseases are defined more specifically than in the past with a focus on their molecular makeup. That is, the genes related to the DNA of the disease and other molecular elements. Precision medicine has vastly improved the ability to diagnose rare inherited diseases; to diagnose and treat cancers; and to aid in diagnosis and management of infectious diseases, dementia and heart disease among many others.
Amy’s story
At Amy’s fifth gene test during her life, performed using the seventh version of specialist software for mutation detection associated with muscle disease, she was finally told which mutation led to her disability.
Some rare neuromuscular diseases are limited to very few families in the world. When only one family member is affected, and particularly if they are the first in the family, the responsible defect in the gene can be extremely difficult to determine among all the normal variations in the human genome.
Through access to global repositories of genomic data, Amy’s specialist has been able to download all known cases of this disease in the world. She has summarised information on the likely health outcomes of other patients and available treatment options or trials.

Amy’s disease is so newly diagnosed that there has been no funded research in this specific area. But there are similarities with other better known muscle disorders. Using international databases, the specialist finds a potential trial applicable to Amy. The trial has shown promise in preventing continued decline of muscle function.
Amy’s mother is relieved she finally has an answer to the cause of her daughter’s disability. Putting a name to it and knowing there are others with this disease comforts her. Of course, knowing potential trials might help stabilise her daughter’s condition leaves her with some hope that continued decline in Amy’s muscle strength is not inevitable.
That night, after putting Amy to bed, Amy’s mother contemplates trying for a second child. There has been a public debate in Australia about preconception screening, which would allow a mother to abort her foetus if it’s known to be carrying a gene mutation that causes a severe debilitating disease. The debate has concluded that preconception screening is allowed under certain circumstances.
Now that Amy’s mutation is known, preconception screening is an option. Amy’s mother will discuss this with her husband in the morning.
Anh’s story
Anh, a 45-year-old web designer, wants to know more about the prognosis and management of his cancer now that he's had the operation to remove it.
Before the operation, he was examined with the latest nuclear-medicine-based imaging technologies. This includes imaging at the molecular level with state-of-the-art scans that have been subsidised through Medicare. Specialist radiologists examined the results using high-resolution smart sensing imaging software to look for any spread of tumour (the software can sense known tumour markers).

Anh had also had his blood examined by molecular pathologists who looked for any tiny bits of tumour DNA circulating in his blood. In 2018, this technology (known as a liquid biopsy) was only just starting out and used in very few places, as it required specialist molecular knowledge. It was purely a research tool, unfunded by Medicare and not approved for use in a diagnostic laboratory setting.
Anh’s treating team used a combination of information to feel reasonably confident there was no evidence of any tumour spread before his operation. Unfortunately, the sensitivity of these tests is still not yet at 100 per cent, so ongoing follow-up will be required.
At the time of the operation, specialist hospital pathologists examined part of Ahn’s lung affected by the tumour. They performed tests that looked at the entire makeup of the tumour, which yielded plenty of information to compare with the world literature and international database for the same tumour, including its specific markers.
Tumour markers are the unique aspects of DNA and proteins that make the tumour “signature”. Drugs can then target and block some of these specific markers to prevent the tumour from progressing, or even to destroy the tumour.
Mutation of the tumour over time and changes in the molecular markers remain a problem. This has been an ongoing area of research, central to government funding policy, for the past 10 years. It takes many years and a large amount of expertise and money from the time of finding a target to developing and trialling drugs.

In 2018, only 10 to 15 per cent of patients with lung cancer had a tumour molecular target that had an available drug that could work on it. In 2030, that rate is much higher.
Anh asks his oncologist what he expects will happen to him in the future. The doctor explains each individual needs to be seen in his own right despite the collective world of data about his tumour. He says the presence of this new gene marker will be fed into a research and trials database to find what is happening in the world in relation to drugs targeting this novel marker.
For now, Anh has a good outlook. The results of the analysis of his lung tumour in the pathology department – which looked at key issues such as the tumour type and size, and whether it's been removed completely or entered small vessels – and the examination of the molecular signature of the tumour are all entered into the diagnostic algorithm based on global data. It's suggested the chances of Anh’s tumour coming back within five years are about 5 to 10 per cent. Pretty low.
The oncologist tells Anh he's free to go back to work. He'll monitor him with regular blood checks aimed at markers for his specific tumour. Now that these are known, the specific test can be individualised to Anh’s tumour. The hand-held screening gadget can send the information straight to the specialist’s office, so he'll be notified automatically in the event of change.
Precision medicine has truly made a difference in the lives of millions of people around the world. While there are still many issues to be fixed, including adequate funding for further research continuing from the new information provided, appropriate drug trial funding and ethical issues, the future is looking brighter.

This article originally appeared on The Conversation.
Catriona McLean does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.





